Virginia Henderson’s Need Theory highlights 14 essential activities that nurses help patients achieve, promoting independence, dignity, and holistic care.
The theory emphasizes meeting physical, psychological, and social needs to improve patient outcomes.
It provides a practical framework for nurses to support recovery by addressing basic functions like breathing, hygiene, and communication.
By fostering patient autonomy, Henderson’s approach ensures individualized and comprehensive care.
In this article, we’ll explore the theory’s core concepts, the 14 fundamental needs, and real-world examples of how it’s applied today.
What You’ve Learned – Virginia Henderson’s Need Theory
- Nursing focuses on promoting independence: Henderson’s theory emphasizes helping patients meet 14 fundamental needs to achieve autonomy and dignity, fostering long-term recovery.
- Holistic care involves addressing more than physical needs: Nurses must support emotional, social, and psychological well-being to ensure comprehensive care and better outcomes.
- The 14 needs guide personalized interventions: By assessing each patient’s unique situation, nurses can tailor interventions that meet specific needs, from basic hygiene to emotional support.
- Collaboration enhances holistic patient care: Interdisciplinary teamwork helps address complex cases, ensuring that every need—physical, psychological, and spiritual—is adequately met.
- Henderson’s theory remains relevant in modern healthcare: Whether in hospital settings, long-term care, or home health, her principles help nurses provide patient-centered, goal-oriented care.
Core Concepts of Virginia Henderson’s Need Theory
Virginia Henderson’s theory is based on the belief that nurses play a key role in helping patients meet fundamental needs they are unable to fulfill on their own.
Her definition of nursing goes beyond treating illness—it focuses on promoting health, recovery, and peaceful death by supporting patient independence.
The Definition of Nursing According to Henderson
Henderson defined nursing as assisting individuals, sick or well, in performing activities that contribute to health, recovery, or a peaceful death—activities they would do independently if they had the necessary strength, will, or knowledge.
Key Insight:
Nursing isn’t just about providing temporary assistance; it’s about guiding patients toward self-care, whenever possible.
The Importance of Patient Independence
Henderson believed that regaining independence was a critical step in the recovery process.
When patients can meet their own needs, they experience improved well-being, dignity, and autonomy.
Nurses act as temporary providers of care but aim to reduce their involvement as patients recover.
Example in Practice:
In rehabilitation settings, nurses encourage patients recovering from strokes to gradually take on tasks such as eating and walking on their own through supportive interventions and exercises.
Think of it as…
Giving someone the tools and confidence to care for themselves, rather than doing everything for them.
The 14 Fundamental Needs
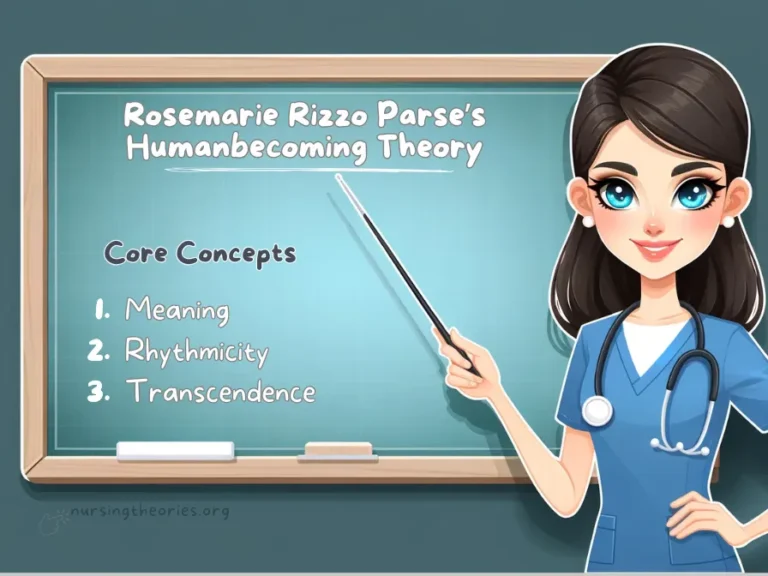
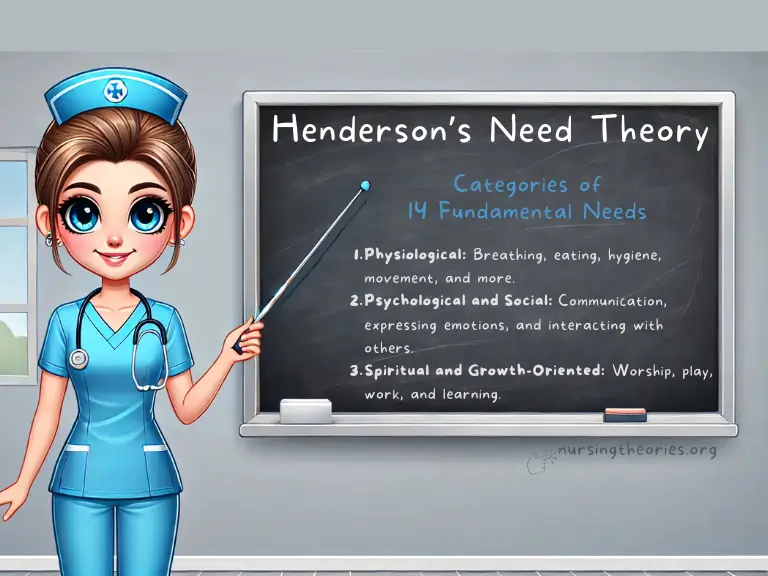
Henderson identified 14 core needs, grouped into categories such as physiological, psychological, social, and spiritual needs.
These form the foundation of her theory and guide nursing interventions across diverse healthcare settings.
Categories of Needs:
- Physiological: Breathing, eating, hygiene, movement, and more.
- Psychological and Social: Communication, expressing emotions, and interacting with others.
- Spiritual and Growth-Oriented: Worship, play, work, and learning.
14 Fundamental Needs Explained with Practical Applications
Henderson’s 14 fundamental needs cover essential aspects of human health, addressing physical, psychological, social, and spiritual well-being.
Nurses play a vital role in assessing which of these needs patients cannot meet on their own and providing support to promote independence and recovery.
i) Physiological Needs
1) Breathing
- Explanation: Adequate oxygen supply is essential for cellular function and life. Nurses ensure that patients with respiratory issues receive proper care.
- Practical Application: Administering oxygen therapy, monitoring oxygen saturation, and assisting patients with airway clearance.
Example: Nurses helping patients with asthma manage their breathing using nebulizers or inhalers.
2) Eating and Drinking
- Explanation: Proper nutrition and hydration are vital for energy and recovery.
- Practical Application: Assessing patients’ nutritional intake and providing feeding assistance when needed.
Example: A nurse ensuring a stroke patient is properly nourished by offering soft foods or assisting with IV fluids if oral intake is inadequate.
3) Elimination
- Explanation: Proper bladder and bowel function is important for removing bodily waste and maintaining balance.
- Practical Application: Monitoring urine output and bowel activity, assisting patients with elimination through catheters or bedpans.
Example: Post-operative patients being monitored for signs of urinary retention or constipation.
4) Movement and Posture
- Explanation: Mobility is essential for circulation, preventing pressure ulcers, and maintaining independence.
- Practical Application: Assisting with walking, positioning, and physical therapy.
Example: Helping a patient ambulate after surgery or ensuring a bedridden patient changes position regularly to avoid bedsores.
5) Sleep and Rest
- Explanation: Proper sleep is necessary for physical and mental recovery.
- Practical Application: Creating restful environments by minimizing noise and managing pain.
Example: Enforcing quiet hours in hospital settings and using relaxation techniques to promote better sleep.
6) Clothing and Body Temperature Regulation
- Explanation: Maintaining a stable body temperature is crucial for metabolic functions and comfort.
- Practical Application: Providing appropriate clothing and controlling the room’s temperature.
Example: Offering warm blankets for patients experiencing chills or providing cool compresses during a fever.
7) Maintaining Hygiene
- Explanation: Personal hygiene helps prevent infections and promotes comfort and self-esteem.
- Practical Application: Assisting patients with bathing, oral hygiene, and skincare routines.
Example: Helping immobile patients maintain skin integrity by regularly cleaning and moisturizing their skin.
8) Avoiding Dangers
- Explanation: Keeping patients safe from injury, infection, and health complications.
- Practical Application: Identifying risks and implementing preventive measures, such as fall prevention protocols.
Example: Nurses installing bedrails for elderly patients at risk of falling and ensuring sterile techniques during wound dressing.
iI) Psychological and Social Needs
9) Communication
- Explanation: Effective communication ensures patients can express their needs and concerns.
- Practical Application: Encouraging verbal and non-verbal communication through devices or gestures when needed.
Example: A nurse using communication boards for patients with speech impairments or non-English speakers.
10) Worship and Spiritual Expression
- Explanation: Spiritual and religious activities provide emotional comfort and meaning.
- Practical Application: Respecting spiritual beliefs and facilitating religious practices when requested.
Example: Organizing chaplain visits or providing prayer spaces for patients seeking spiritual support.
iII) Needs Related to Achievement and Growth
11) Work and Play
- Explanation: Engaging in purposeful activities helps patients maintain mental stimulation and physical function.
- Practical Application: Encouraging activities that match a patient’s abilities and interests.
Example: A long-term care nurse organizing recreational activities like gardening or crafts to boost morale and engagement.
12) Learning
- Explanation: Patients need to understand their conditions and participate in their care plans.
- Practical Application: Educating patients about medications, treatments, and lifestyle adjustments.
Example: Teaching a diabetic patient how to monitor blood sugar levels and administer insulin.
13) Expression of Emotions
- Explanation: Addressing emotional well-being is vital for mental health and recovery.
- Practical Application: Providing emotional support, listening to patients’ concerns, and facilitating therapeutic interventions.
Example: A nurse offering counseling or referring a patient to a mental health professional when needed.
14) Sense of Achievement
- Explanation: Encouraging small, achievable goals improves confidence and motivation.
- Practical Application: Setting personalized recovery milestones to promote progress.
Example: Celebrating milestones, such as a patient regaining the ability to walk independently after physical therapy.
Real-World Examples of Virginia Henderson’s Need Theory in Practice
Case Study 1: Rehabilitation Nursing
Scenario: A 65-year-old male patient recovering from a stroke has limited mobility, speech difficulties, and partial paralysis.
His primary goal is to regain independence in daily activities.
Application of Henderson’s Needs:
- Movement and Posture: Nurses assist the patient with physical therapy exercises and help him sit or walk with support.
- Communication: Nurses use communication boards to help the patient express basic needs and emotions while speech therapy is ongoing.
- Elimination and Hygiene: Nurses provide support with toileting and hygiene while gradually encouraging the patient to regain control.
Outcome: With consistent interventions, the patient regains partial mobility, begins speaking short sentences, and independently performs hygiene tasks, reflecting gradual progress toward independence.
Case Study 2: Long-Term Care Facilities
Scenario: An elderly woman with dementia residing in a long-term care facility requires assistance with daily activities, emotional support, and memory-related interventions.
Application of Henderson’s Needs:
- Hygiene and Safety: Nurses assist with daily bathing, dressing, and ensuring the patient’s room is free of hazards to prevent falls.
- Nutrition: The nursing staff monitors her dietary intake and encourages meals high in nutrients to maintain strength.
- Social Interaction: The patient is involved in group activities, such as music therapy and art classes, to stimulate cognitive function and reduce loneliness.
Outcome: The patient maintains good physical health, experiences fewer episodes of agitation, and shows improved mood through regular social engagement and emotional support.
Case Study 3: Pediatric Care
Scenario: A 6-year-old boy is hospitalized for a broken leg after a playground accident.
He is anxious about medical procedures and has difficulty sleeping due to pain.
Application of Henderson’s Needs:
- Pain Management and Sleep: Nurses provide pain relief through medication and comfort measures, such as repositioning and distraction techniques.
- Play and Learning: Child life specialists collaborate with nurses to provide play activities that promote emotional well-being and distract the child from medical stress.
- Emotional Support: Nurses address the child’s fears by explaining procedures using age-appropriate language and involving his parents in the care plan.
Outcome: The child becomes more cooperative during medical treatments and sleeps better with pain management, resulting in a quicker recovery and reduced anxiety.
Modern Implications of Virginia Henderson’s Need Theory
Patient-Centered Care
Modern nursing emphasizes personalized care, which closely reflects Henderson’s belief in addressing each patient’s unique needs.
Today, patient-centered models integrate her concepts by creating individualized care plans that promote independence and holistic recovery.
Example:
A care plan for a patient recovering from surgery may involve addressing physical needs, such as pain management and mobility, alongside emotional needs, such as coping with anxiety.
Key Insight:
When nurses create care plans that address Henderson’s 14 fundamental needs, they help foster autonomy, dignity, and optimal recovery.
Think of it as…
Giving a patient both the crutches and the emotional support they need, so they can take their first steps toward independence.
Interdisciplinary Collaboration
Henderson’s theory encourages collaboration between nurses, doctors, nutritionists, physical therapists, and other healthcare professionals to meet comprehensive patient needs.
As healthcare becomes more team-oriented, her holistic approach is vital in ensuring every aspect of a patient’s health is addressed.
Example:
A patient recovering from a spinal injury may require interventions from various specialists:
- Nurses for hygiene, mobility, and emotional support
- Physical therapists for mobility exercises
- Dietitians for nutritional planning
Key Insight:
When all members of a healthcare team work together using Henderson’s holistic approach, patients experience seamless, well-coordinated care.
Think of it as…
A symphony, where every specialist plays their part, creating a harmonious and effective recovery process.
Application in Community and Home Health Settings
Henderson’s theory is particularly valuable in community and home healthcare, where patients often need support with everyday activities.
Nurses in these settings help patients transition from hospital care to independent living by gradually reducing their involvement as patients regain function.
Example:
A home health nurse assisting an elderly patient recovering from hip surgery may initially provide help with mobility, hygiene, and meal preparation but gradually encourage the patient to take on these activities independently.
Key Insight:
By fostering independence within community settings, nurses empower patients to manage their health outside clinical environments, reducing readmission rates.
Think of it as…
A safety net that supports patients just long enough for them to regain balance on their own.
Challenges in Implementing virginia Henderson’s Theory Today
Staffing Shortages and Time Constraints
One of the primary challenges in modern healthcare is the shortage of nurses and increased patient loads, which can limit the time available to address all 14 needs comprehensively.
Nurses often have to prioritize immediate physical needs, leaving little time for addressing emotional, social, and growth-related needs.
Example:
A nurse in a busy emergency department may focus on administering medications, stabilizing vital signs, and performing critical procedures, while needs like communication or emotional support may be overlooked.
Key Insight:
While time constraints are a reality, small but meaningful interactions can still address emotional and social needs.
Even brief moments of active listening can make a difference.
Think of it as…
Watering a plant regularly—even if only a little—ensures that growth continues without being neglected entirely.
Complex Patient Conditions
Patients with multiple chronic conditions, mental health issues, or disabilities often present complex cases where several needs overlap, making it difficult to address them all effectively.
Example:
A patient with diabetes and depression may require attention to physical needs (e.g., blood glucose monitoring) and psychological support.
Managing both simultaneously can be challenging, especially when their conditions interact (e.g., poor mental health affecting diet adherence).
Key Insight:
Nurses should collaborate with interdisciplinary teams to divide responsibilities, ensuring that no aspect of the patient’s care is neglected.
Think of it as…
Building a bridge with multiple supporting beams, where each beam represents different professionals working together to support the patient’s overall health.
Balancing Technology and Hands-On Care
Technological advances in healthcare, such as electronic health records (EHRs), monitoring devices, and automated medication systems, have streamlined nursing workflows.
However, they can also create barriers to the hands-on, personalized care that Henderson emphasized.
Example:
Nurses may spend more time documenting patient care and managing devices than interacting directly with patients, potentially diminishing the human connection and emotional support.
Key Insight:
Integrating technology into nursing workflows should enhance, not replace, face-to-face interactions.
Nurses can use tech tools to free up time for meaningful patient engagement.
Think of it as…
Using a GPS to find the quickest route—not to replace the journey but to ensure you reach your destination more efficiently.
virginia Henderson’s Need Theory Quiz
1) What is the main goal of Henderson’s Need Theory?
a) Provide treatment and medication
b) Achieve patient independence
c) Conduct regular diagnostic tests
d) Minimize hospital stays
2) Which of the following is one of the 14 needs outlined in Henderson’s theory?
a) Psychological counseling
b) Ventilation monitoring
c) Proper elimination
d) Continuous lab testing
3) What is a practical way to address the communication need of a stroke patient who cannot speak?
a) Provide a tablet with games
b) Offer speech therapy immediately
c) Use communication boards and non-verbal gestures
d) Encourage the patient to write down their thoughts
4) Why does Henderson’s theory emphasize regaining independence?
a) To reduce hospital stays and minimize costs
b) To improve patient dignity and long-term recovery
c) To allow nurses to focus on other patients
d) To meet insurance criteria for discharge
5) How can nurses meet a patient’s hygiene need when they are bedridden?
a) Encourage the patient to clean themselves
b) Provide brief cleaning once daily
c) Perform bed baths and change linens regularly
d) Focus only on essential hygiene, like oral care
virginia Henderson’s Need Theory Quiz Answers with Rationale
1) Correct Answer: b) Achieve patient independence
Rationale: Henderson’s theory focuses on helping patients regain independence in performing daily activities, which improves their dignity, recovery, and overall quality of life.
2) Correct Answer: c) Proper elimination
Rationale: Proper elimination is one of the 14 physiological needs identified by Henderson, essential for maintaining homeostasis and preventing complications like urinary tract infections or constipation.
3) Correct Answer: c) Use communication boards and non-verbal gestures
Rationale: Henderson emphasized communication as a fundamental need.
For patients unable to speak, alternative methods like boards and gestures help maintain effective communication and emotional support.
4) Correct Answer: b) To improve patient dignity and long-term recovery
Rationale: By promoting independence, Henderson’s theory ensures that patients regain control over their lives, fostering a sense of dignity and improved long-term health outcomes.
5) Correct Answer: c) Perform bed baths and change linens regularly
Rationale: Maintaining hygiene prevents infections, promotes skin integrity, and enhances patient comfort, which is crucial in Henderson’s holistic approach to nursing care.
Questions and Answers of Virginia Henderson’s Need Theory
Q1) What is the primary focus of Henderson’s Need Theory?
A: Helping patients achieve independence by meeting their physical, emotional, and social needs.
Q2) How can nurses assess which needs a patient requires help with?
Through comprehensive assessments during admission, continuous monitoring, and open communication with patients.
Q3) Why is patient independence emphasized in Henderson’s theory?
Independence fosters long-term recovery, dignity, and a sense of control over one’s life.
Q4) How does Henderson’s theory support chronic care management?
A: By addressing ongoing needs such as nutrition, mobility, and emotional well-being to promote sustainable health outcomes.
Q5) What role does interdisciplinary collaboration play in Henderson’s theory?
A: Collaboration ensures that different professionals meet diverse patient needs, from physical therapy to emotional support, promoting holistic care.
Conclusion
Virginia Henderson’s Need Theory has stood the test of time, influencing nursing practice worldwide by emphasizing independence, dignity, and holistic care.
By addressing 14 fundamental needs—spanning physiological, emotional, and social domains—nurses can create personalized care plans that improve patient outcomes and foster long-term well-being.
In today’s healthcare settings, Henderson’s theory continues to be an essential framework for patient-centered care.
Whether applied in acute hospital settings, long-term care, or community nursing, it empowers nurses to act as caregivers, educators, and advocates, helping patients regain autonomy and control over their health.
Final Reflective Question:
How can you apply Henderson’s 14 fundamental needs to enhance patient care and promote independence in your nursing practice?