Sister Callista Roy’s Roy Adaptation Model (RAM) is a foundational nursing theory that views patients as adaptive systems constantly interacting with their environment.
Developed in the 1970s, the model emphasizes the importance of adaptation as a key process in maintaining physical, emotional, and social well-being.
According to Roy, patients experience health challenges as stimuli that trigger adaptive responses, which can either promote recovery or lead to maladaptation.
Nurses play a vital role in this process by assessing a patient’s adaptive behaviors and intervening to promote positive responses.
This comprehensive guide will provide step-by-step insights into applying the Roy Adaptation Model in clinical practice, with real-world examples to illustrate its practical applications.
What You’ve Learned – Roy Adaptation Model
- Patients are adaptive systems: The Roy Adaptation Model views patients as constantly adjusting to changes in their internal and external environments.
- Four adaptive modes guide assessment: Nurses assess patients’ adaptation through the physiological, self-concept, role function, and interdependence modes.
- Stimuli influence adaptation: Focal, contextual, and residual stimuli shape how patients respond to health challenges, and managing these stimuli is crucial to promoting positive adaptation.
- The six-step nursing process: RAM follows a structured process, from assessing patient behavior to evaluating nursing interventions, ensuring individualized care plans are developed and refined.
- Applicable across healthcare settings: The model is effective in acute care, chronic illness management, rehabilitation, and end-of-life care, making it a versatile tool for holistic nursing practice.
Core Concepts of the Roy Adaptation Model
The Roy Adaptation Model revolves around the idea that individuals are adaptive beings who respond to internal and external stimuli.
When confronted with health challenges, the body and mind strive to adapt, either successfully or unsuccessfully.
Nurses assess this adaptation process and intervene when needed to promote positive outcomes.
1) Adaptation as the Central Focus
Adaptation is at the heart of Roy’s model, emphasizing how individuals respond to stimuli and adjust their behavior to maintain health and well-being.
Adaptation is a continuous process and can occur at the physical, emotional, and social levels.
Why It’s Important: When adaptation is successful, patients regain balance and move toward health.
When maladaptation occurs, nursing interventions are required to help them recover or improve their condition.
Example:
A patient undergoing chemotherapy may face fatigue, nausea, and emotional distress.
Adaptation involves developing coping mechanisms like rest periods, anti-nausea management, and emotional support.
Key Insight:
Nurses act as facilitators, helping patients navigate through the adaptation process by addressing barriers and promoting positive change.
Think of it as…
Helping a plant grow under different weather conditions by adjusting water, sunlight, and nutrients to support optimal growth.
2) The Four Adaptive Modes
Roy’s model classifies adaptation into four key modes that nurses use to assess how well patients are coping and where interventions may be needed.
- Physiological Mode:
- Focuses on the body’s physical and biological processes, such as breathing, circulation, and metabolism.
- Example: Managing pain and fatigue in post-operative patients through medication and mobility exercises.
- Self-Concept Mode:
- Involves the patient’s perception of themselves, including body image, self-esteem, and emotional well-being.
- Example: Providing support to a breast cancer survivor who is coping with changes to their body image after a mastectomy.
- Role Function Mode:
- Relates to the roles patients fulfill in life, such as being a parent, spouse, or employee, and how illness affects these roles.
- Example: Helping a patient with chronic arthritis adapt to their work responsibilities through physical therapy and ergonomic support.
- Interdependence Mode:
- Focuses on the patient’s interactions with others, including relationships with family, friends, and caregivers.
- Example: Ensuring that a patient in long-term care has adequate emotional and social support from loved ones and staff.
Key Insight:
Assessing these four modes provides a holistic view of the patient’s overall well-being and identifies specific areas where nursing interventions are needed.
Think of it as…
A four-legged chair—if one leg is unstable, the entire chair becomes imbalanced, requiring attention to restore stability.
3) Stimuli Affecting Adaptation
Stimuli refer to the internal and external factors that trigger adaptive responses.
Roy categorizes stimuli into three types:
- Focal Stimuli:
- The immediate or primary issue affecting the patient’s adaptation.
- Example: A broken leg causing pain and limited mobility.
- Contextual Stimuli:
- Environmental or background factors that influence the patient’s response.
- Example: The patient’s financial stress or lack of family support affecting their recovery.
- Residual Stimuli:
- Indirect or previously unrecognized factors that may affect adaptation.
- Example: A past trauma that influences the patient’s emotional response to their current condition.
Key Insight:
Managing stimuli is essential for promoting positive adaptation.
Nurses focus on reducing negative stimuli and enhancing supportive factors to achieve better outcomes.
Think of it as…
Adjusting the conditions of a greenhouse—temperature, light, and humidity—to ensure plants grow and thrive.
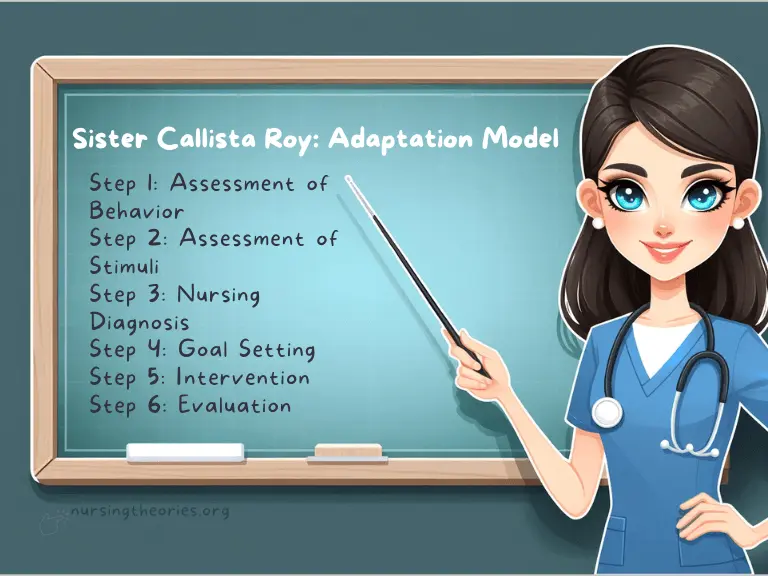
The Six-Step Nursing Process in the Roy Adaptation Model
The Roy Adaptation Model guides nurses through a structured six-step process, ensuring that interventions are tailored to address the specific needs of patients and promote positive adaptation.
Step 1: Assessment of Behavior
In this step, nurses assess the patient’s behavior in each of the four adaptive modes (physiological, self-concept, role function, and interdependence) to determine how well they are coping.
Key Questions to Ask:
- Is the patient showing physical signs of distress, such as pain or fatigue?
- How does the patient feel about their current health status or body image?
- Are there any changes in the patient’s role or responsibilities due to illness?
- Does the patient have adequate emotional or social support?
Example:
A patient with heart failure may exhibit shortness of breath (physiological), anxiety about their condition (self-concept), difficulty fulfilling work responsibilities (role function), and isolation from family (interdependence).
Step 2: Assessment of Stimuli
Nurses identify the focal, contextual, and residual stimuli affecting the patient’s behavior and adaptation.
Understanding these stimuli helps in planning appropriate interventions.
Key Considerations:
- What is the main issue the patient is facing (focal stimulus)?
- Are there any environmental or background factors contributing to the issue (contextual stimuli)?
- Could past experiences or unrecognized factors (residual stimuli) be influencing the patient’s current behavior?
Example:
For a patient experiencing post-surgical pain, the focal stimulus is the surgical site pain, while the contextual stimuli may include a lack of sleep or support.
Residual stimuli could involve a previous negative experience with surgery.
Step 3: Nursing Diagnosis
Based on the assessment, nurses develop a nursing diagnosis to identify maladaptive behaviors and define specific problems that require intervention.
Key Question:
What is preventing the patient from adapting effectively, and how can nursing care address it?
Example Diagnosis:
- Ineffective coping related to fear of post-surgical complications as evidenced by anxiety, insomnia, and withdrawal from social interactions.
Step 4: Goal Setting
Nurses establish clear, measurable goals aimed at promoting positive adaptation.
These goals should be realistic and time-bound.
Example Goals:
- The patient will verbalize reduced anxiety within 48 hours of nursing intervention.
- The patient will perform light exercises to improve mobility within three days.
- The patient will participate in family support activities within one week.
Key Insight:
Setting achievable goals ensures that progress can be measured and adjustments made when necessary.
Think of it as…
Creating a personalized roadmap that guides both the patient and the nurse toward recovery.
step 5: Intervention
Nurses implement interventions tailored to managing stimuli and promoting adaptive behaviors.
Interventions may include physical care, emotional support, patient education, or environmental adjustments.
Example Interventions:
- Administering pain medication and encouraging rest to address physiological needs.
- Providing counseling or relaxation exercises to reduce anxiety and improve self-concept.
- Coordinating with occupational therapists to help patients adapt to new roles or limitations.
Step 6: Evaluation
Nurses evaluate whether the interventions were effective in promoting adaptation and achieving the set goals.
If the goals are not met, the care plan is revised accordingly.
Evaluation Criteria:
- Has the patient shown improvement in physical symptoms or emotional well-being?
- Are the patient’s relationships or role functions returning to normal?
- Is the patient developing adaptive coping mechanisms?
Example:
If a post-surgical patient successfully reports reduced pain, improved mobility, and active participation in support groups, the nursing interventions can be considered effective.
Key Insight:
Continuous evaluation ensures that nursing care remains dynamic and responsive to the patient’s changing needs.
Think of it as…
Checking the GPS during a trip to ensure you’re on the right path and making course corrections if necessary.
Real-World Applications of the Roy Adaptation Model
The Roy Adaptation Model can be applied in various healthcare settings, from acute care units to long-term care facilities.
By addressing physical, emotional, and social factors, nurses help patients adapt to their health challenges and improve overall well-being.
Here are some real-world case studies to demonstrate its practical use.
Case Study 1: Post-Traumatic Rehabilitation
Scenario:
A 28-year-old male athlete sustained a spinal cord injury in a car accident, resulting in partial paralysis.
He struggles with physical limitations, emotional distress, and the loss of his athletic role.
Application of the Roy Adaptation Model:
- Physiological Mode: Physical therapy and mobility exercises help improve his strength and prevent complications like muscle atrophy.
- Self-Concept Mode: Counseling sessions address feelings of grief, loss of identity, and body image concerns.
- Role Function Mode: Nurses work with him to explore new roles and responsibilities outside of sports, such as coaching.
- Interdependence Mode: Social workers and family members provide emotional and social support.
Outcome:
With an individualized care plan, the patient shows improvement in mobility, gains confidence, and embraces his new role as a sports mentor.
Case Study 2: Chronic Illness Management
Scenario:
A 60-year-old woman with chronic kidney disease (CKD) is undergoing dialysis three times a week.
She experiences fatigue, depression, and a sense of dependency due to role changes within her family.
Application of the Roy Adaptation Model:
- Physiological Mode: Dietary interventions, regular monitoring of lab values, and managing fatigue.
- Self-Concept Mode: Psychosocial support to address feelings of inadequacy and promote self-esteem.
- Role Function Mode: Helping her redefine her role within the family by involving her in non-physical household tasks.
- Interdependence Mode: Encouraging participation in support groups for CKD patients.
Outcome:
The patient develops coping strategies, adheres to her treatment plan, and regains a sense of purpose within her family and community.
Case Study 3: Pediatric Care
Scenario:
A 10-year-old child with asthma frequently misses school due to symptoms and is struggling academically and socially.
Application of the Roy Adaptation Model:
- Physiological Mode: Asthma management through medication, breathing exercises, and regular monitoring.
- Self-Concept Mode: Addressing feelings of isolation and reduced self-worth due to missed school and peer interaction.
- Role Function Mode: Working with teachers to create a flexible academic plan to help the child catch up on schoolwork.
- Interdependence Mode: Engaging the family in asthma education and creating a supportive home environment.
Outcome:
The child experiences fewer asthma episodes, gains confidence, and improves both academic performance and social interactions.
Key Insight:
Real-world applications demonstrate that addressing adaptation holistically—physically, emotionally, and socially—leads to sustainable improvements in health outcomes.
Think of it as…
Building a sturdy bridge over rough waters by reinforcing multiple support points to ensure it holds steady.
Modern Implications of the Roy Adaptation Model
The Roy Adaptation Model remains highly relevant in today’s healthcare environments, supporting holistic, patient-centered care.
It adapts to evolving healthcare needs, including the management of chronic illnesses, mental health conditions, and end-of-life care.
The following modern implications illustrate its enduring impact.
Importance in Holistic Nursing
Roy’s model emphasizes treating the whole person—physically, emotionally, socially, and spiritually.
This holistic approach is especially important in complex cases where multiple factors influence recovery.
Example:
In cancer care, nurses use the four adaptive modes to address physical symptoms, emotional distress, role disruptions within the family, and the need for social support.
By integrating all aspects of the patient’s well-being, care becomes comprehensive and personalized.
Key Insight:
Holistic care promotes long-term health by addressing underlying emotional or social factors, not just physical symptoms.
Think of it as…
Treating the entire tree, from its roots to its leaves, to ensure healthy growth rather than just trimming its branches.
Adaptation in Chronic Disease and End-of-Life Care
Patients with chronic conditions or those receiving palliative care face ongoing adaptation challenges.
The Roy Adaptation Model helps nurses manage long-term care while focusing on patient dignity, comfort, and quality of life.
Example:
A terminally ill patient with advanced lung disease may experience adaptation issues related to breathlessness (physiological), fear of death (self-concept), changing family roles (role function), and emotional dependence on caregivers (interdependence).
Application:
Nurses help manage symptoms, provide emotional support, and involve the family in care decisions to ease the patient’s transition and improve quality of life.
Key Insight:
Adaptation isn’t just about recovery—it also involves accepting and coping with life-altering conditions in a supportive environment.
Think of it as…
Guiding a ship through turbulent waters while ensuring it stays afloat and maintains direction.
Interdisciplinary Collaboration
The Roy Adaptation Model integrates seamlessly with interdisciplinary teams, making it ideal for complex care environments like hospitals and rehabilitation centers.
Nurses collaborate with doctors, physical therapists, social workers, and mental health professionals to address all aspects of adaptation.
Example:
A stroke patient may require speech therapy (addressing physiological adaptation), counseling (self-concept adaptation), role reintegration planning with occupational therapists, and family support coordination.
Key Insight:
Collaboration maximizes care outcomes by leveraging the expertise of multiple disciplines to address various adaptation challenges.
Think of it as…
A symphony where each instrument contributes to a harmonious performance, ensuring all aspects of the patient’s health are considered.
Challenges and Limitations of the Roy Adaptation Model
While the Roy Adaptation Model is a valuable framework, its practical application can present challenges.
Recognizing these limitations enables nurses to address them proactively and make adjustments where necessary.
Complexity of the Assessment Process
The model’s emphasis on evaluating stimuli, adaptive modes, and behaviors can be time-consuming and complex, particularly in high-stress, fast-paced environments like emergency departments.
Example:
In an ICU setting, nurses may struggle to conduct thorough assessments of all four adaptive modes while managing acute medical needs.
Key Insight:
Streamlining assessments and prioritizing critical modes can help nurses address immediate needs without neglecting the holistic perspective.
Think of it as…
Focusing on essential repairs first when fixing a car but scheduling follow-up checks to ensure full functionality.
individual Differences in Adaptation
Patients have varying adaptive capacities, influenced by factors like age, cultural background, and prior experiences.
What works for one patient may not be effective for another, making it difficult to standardize interventions.
Example:
An older patient with diabetes may adapt slowly to lifestyle changes, requiring gradual, supportive interventions, while a younger patient may show quicker progress.
Key Insight:
Nurses should customize care plans and be flexible, regularly reassessing and adjusting interventions based on the patient’s progress.
Think of it as…
Tailoring a fitness program where some participants require a slower pace while others can handle more intense activities.
Balancing Physical and Psychological Needs
Nurses often face challenges in balancing the management of physical symptoms with the need to address emotional and social adaptation, particularly when resources are limited.
Example:
A cancer patient may need both pain management and counseling for depression, but limited nursing time may prioritize physical care over emotional needs.
Key Insight:
Collaboration with interdisciplinary teams and efficient time management help ensure that all aspects of patient care are addressed.
Think of it as…
Allocating water evenly to all plants in a garden to ensure every part thrives, not just the ones in immediate view.
Resource and Staffing Constraints
In healthcare settings with limited resources or staffing shortages, it may be challenging to follow the comprehensive steps of the Roy Adaptation Model consistently.
Example:
A nurse on a busy hospital ward may only have time to address critical physiological needs, delaying interventions for self-concept or role function adaptation.
Key Insight:
Even small interventions that address immediate stimuli can create positive effects, and follow-up care can help address long-term adaptation needs.
Think of it as…
Applying temporary fixes to prevent further damage while planning for long-term repairs.
Roy Adaptation Model Quiz
- What is the primary focus of the Roy Adaptation Model?
a) Disease prevention
b) Patient adaptation to internal and external changes
c) Medical treatment of chronic conditions
d) Immediate symptom relief
- Which of the following is NOT one of the four adaptive modes in the Roy Adaptation Model?
a) Physiological mode
b) Cognitive-behavioral mode
c) Role function mode
d) Self-concept mode
- How do residual stimuli influence a patient’s adaptation?
a) They directly trigger a patient’s response
b) They are unrecognized factors that may indirectly affect adaptation
c) They have no impact on the adaptation process
d) They are the primary focus of nursing intervention
- What is the purpose of the goal-setting step in the nursing process of the Roy Adaptation Model?
a) To identify patient deficiencies
b) To provide specific, measurable outcomes for adaptive progress
c) To complete nursing documentation
d) To determine the length of hospital stay
- In the Roy Adaptation Model, which stimulus is described as the immediate issue affecting the patient’s adaptation?
a) Focal stimulus
b) Contextual stimulus
c) Residual stimulus
d) Secondary stimulus
Roy Adaptation Model Quiz Answers with Rationale
- Correct Answer: b) Patient adaptation to internal and external changes
Rationale: The Roy Adaptation Model focuses on how individuals respond to stimuli and adapt to maintain health and well-being. - Correct Answer: b) Cognitive-behavioral mode
Rationale: The four adaptive modes in the model are physiological, self-concept, role function, and interdependence. Cognitive-behavioral mode is not part of this framework. - Correct Answer: b) They are unrecognized factors that may indirectly affect adaptation
Rationale: Residual stimuli are factors that are not immediately obvious but can influence how patients adapt to their situation. - Correct Answer: b) To provide specific, measurable outcomes for adaptive progress
Rationale: Setting clear goals ensures that patient progress can be measured and interventions adjusted as needed to promote adaptation. - Correct Answer: a) Focal stimulus
Rationale: The focal stimulus is the immediate or primary issue affecting the patient’s adaptation, such as pain, illness, or injury.
Questions and Answers of Roy Adaptation Model
- Q: What is the primary role of a nurse using the Roy Adaptation Model?
A: To assess and promote positive adaptation by addressing maladaptive behaviors and managing stimuli. - Q: How do contextual stimuli influence adaptation?
A: Contextual stimuli are background factors, such as the patient’s environment or family support, that influence their response to the focal stimulus. - Q: How can nurses address maladaptation in the self-concept mode?
A: By providing emotional support, counseling, and education to help patients build self-esteem and cope with body image changes or role shifts. - Q: What role does interdisciplinary collaboration play in the Roy Adaptation Model?
A: It ensures that various aspects of the patient’s adaptation, such as physical and emotional needs, are addressed through comprehensive care. - Q: Why is continuous evaluation important in the nursing process?
A: Continuous evaluation helps nurses determine the effectiveness of interventions and make necessary adjustments to improve patient outcomes.
Conclusion
The Sister Callista Roy’s Roy Adaptation Model offers a comprehensive approach to patient care, focusing on how individuals adapt to changing health conditions and environments.
By assessing adaptive behaviors across the four modes—physiological, self-concept, role function, and interdependence—nurses can provide targeted interventions that promote recovery and long-term well-being.
This model’s emphasis on holistic, individualized care ensures that both physical and emotional needs are met, making it highly applicable in various healthcare settings.
As healthcare evolves, the Sister Callista Roy’s RAM continues to provide a structured, adaptable framework for nurses to help patients navigate life’s challenges and achieve positive outcomes.
Its interdisciplinary nature and focus on collaboration make it essential in addressing complex health needs.
Final Reflective Question: How can you apply the Roy Adaptation Model to balance both short-term recovery goals and long-term adaptation in your nursing practice?