Developed by three distinguished nursing theorists—Nancy Roper, Winifred Logan, and Alison Tierney—the Roper-Logan-Tierney Model focuses on holistic, patient-centered care through the assessment of Activities of Daily Living (ADLs).
This framework addresses not only a patient’s physical and medical needs but also the psychological, social, and environmental factors affecting their overall well-being.
In this, you will learn how the Roper-Logan-Tierney Model helps nurses deliver holistic, patient-centered care through real-world applications.
What You’ve Learned – Roper-Logan-Tierney Model of Nursing
- The 12 ADLs form the foundation of comprehensive nursing assessment, guiding care planning and implementation.
- Nurses assess how biological, psychological, and environmental factors affect a patient’s ability to perform ADLs.
- Individualized care plans focus on both immediate needs and long-term independence.
- The lifespan approach ensures interventions are adapted to developmental stages and age-specific requirements.
- Interdisciplinary collaboration enhances care outcomes and holistic patient recovery.
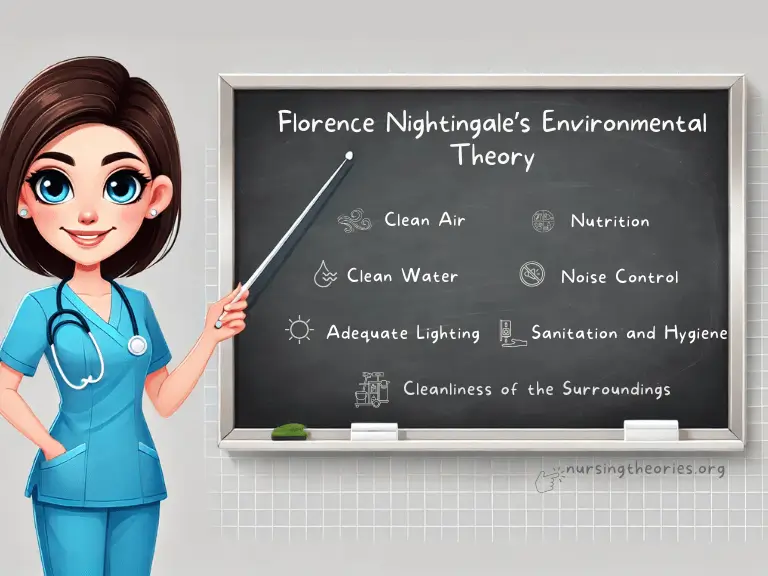
Core Concepts of the Roper-Logan-Tierney Model of Nursing
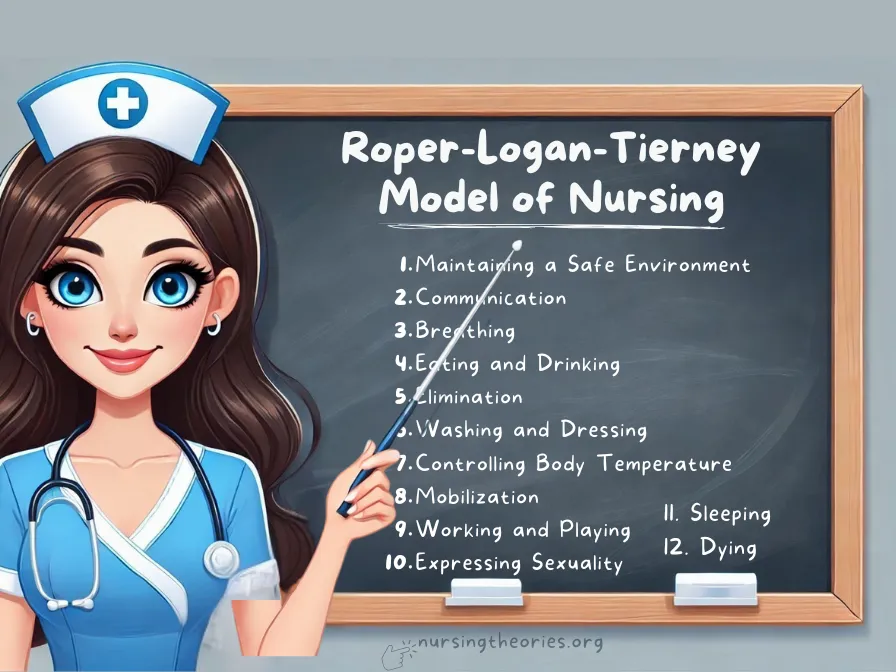
This model is built on the 12 Activities of Daily Living (ADLs), which serve as a guide for identifying a patient’s strengths, limitations, and needs.
1) Activities of Daily Living (ADLs) as the Core of Patient Assessment
The Roper-Logan-Tierney Model revolves around 12 Activities of Daily Living (ADLs), which provide the framework for assessing a patient’s current abilities and planning interventions.
These activities cover fundamental physical, psychological, and social needs, reflecting how patients interact with their environment.
The 12 Activities of Daily Living (ADLs) identified in Roper-Logan-Tierney Model of Nursing are:
I) Maintaining a Safe Environment
Ensuring patients have a living environment free of hazards that could lead to injury or compromise health.
This involves assessing safety measures such as fall prevention and accessibility.
- Example: A nurse identifies fall risks in the home of an elderly patient, recommending grab bars and non-slip mats.
- Key Insight: Safety assessments reduce the risk of injury and enhance patient independence.
- Think of it as… Building a safety net to catch issues before they escalate.
II) Communicating
Assessing a patient’s ability to express needs, share information, and interact effectively with others.
- Example: A patient recovering from a stroke is assessed for speech therapy needs due to difficulties articulating words.
- Key Insight: Effective communication allows patients to express discomfort, participate in care decisions, and seek support.
- Think of it as… Maintaining a two-way radio—clear communication ensures proper coordination and care.
III) Breathing
Evaluating respiratory function and ensuring that patients can maintain adequate oxygen levels.
- Example: A nurse monitors the breathing patterns of a COPD patient and provides breathing exercises to improve lung function.
- Key Insight: Proper breathing assessments help prevent complications, such as respiratory distress.
- Think of it as… Keeping the engine of a car well-maintained—adequate oxygen fuels the body’s performance.
IV) Eating and Drinking
Assessing a patient’s ability to consume food and fluids while ensuring proper nutrition and hydration.
- Example: A cancer patient experiencing nausea and appetite loss is referred to a dietitian for nutritional support.
- Key Insight: Adequate nutrition and hydration are critical to recovery and maintaining bodily functions.
- Think of it as… Refueling a car—without the right fuel, the body cannot function optimally.
V) Eliminating Waste
Monitoring a patient’s ability to manage bladder and bowel function, including incontinence or constipation concerns.
- Example: A post-operative patient is assessed for urinary retention and given a catheter if necessary.
- Key Insight: Maintaining proper elimination supports physical comfort and prevents complications such as infections.
- Think of it as… Clearing waste regularly to keep the system running smoothly and efficiently.
VI) Personal Cleansing and Dressing
Assessing a patient’s ability to maintain personal hygiene and dress independently.
- Example: A patient with limited hand mobility after surgery is provided with adaptive tools for dressing and grooming.
- Key Insight: Good hygiene and appropriate dressing improve self-esteem and prevent infections.
- Think of it as… Maintaining the exterior of a house—cleanliness contributes to overall well-being.
VII) Controlling Body Temperature
Ensuring the patient can maintain a stable body temperature through appropriate clothing, shelter, or medical intervention.
- Example: A nurse monitors a hypothermic patient and adjusts blankets and room temperature to restore normal body heat.
- Key Insight: Body temperature regulation is essential for cellular functions and recovery.
- Think of it as… Adjusting the thermostat—keeping it at the optimal setting ensures comfort and function.
VIII) Mobilizing
Evaluating a patient’s ability to move, including walking, sitting, and repositioning themselves.
- Example: A patient recovering from knee surgery is given mobility exercises and assistive devices.
- Key Insight: Maintaining mobility prevents complications like muscle atrophy and bedsores while promoting independence.
- Think of it as… Keeping a bicycle moving—mobility keeps the body functioning smoothly.
IX) Working and Playing
Assessing a patient’s ability to participate in work, leisure activities, and social interactions, which contribute to mental and emotional well-being.
- Example: A nurse works with a recovering stroke patient to reintegrate hobbies and work tasks into their routine.
- Key Insight: Engagement in meaningful activities promotes emotional resilience and recovery.
- Think of it as… Balancing work and play—a well-rounded life supports overall health.
X) Expressing Sexuality
Evaluating how health conditions impact a patient’s sense of identity, intimacy, and sexual well-being.
- Example: A cancer survivor experiencing body image issues after surgery is provided counseling to help restore confidence.
- Key Insight: Addressing sexuality ensures that patients maintain a healthy self-image and fulfilling relationships.
- Think of it as… Nurturing a flower—emotional well-being requires attention and care.
XI) Sleeping
Ensuring patients achieve restful sleep, which is essential for physical and mental recovery.
- Example: A patient recovering from surgery receives pain management and relaxation techniques to promote sleep.
- Key Insight: Sleep allows the body to heal and enhances cognitive function.
- Think of it as… Charging a phone overnight—rest recharges the body for the next day.
XII) Dying
Providing physical, emotional, and spiritual support during the end-of-life stage.
This includes ensuring comfort and dignity in death.
- Example: A terminally ill patient receives palliative care focused on pain management, emotional support, and spiritual guidance.
- Key Insight: Addressing the dying process holistically ensures that patients experience dignity and peace.
- Think of it as… Helping a loved one cross the finish line—ensuring comfort during the final stage of life.
2) Factors Influencing ADLs
The model identifies five influencing factors—biological, psychological, sociocultural, environmental, and politicoeconomic—that affect the patient’s ability to perform ADLs.
Core Principle: Understanding the interaction between these factors ensures nursing interventions are adaptable and patient-centered.
- Example: A patient recovering from surgery may face psychological barriers, such as fear of pain, that prevent them from engaging in physical therapy.
- Key Insight: Recognizing and addressing influencing factors helps nurses reduce barriers and foster cooperation.
- Think of it as… Adjusting the settings of a machine to ensure optimal performance—each factor matters.
3) Lifespan Approach to Nursing Care
The model incorporates a lifespan approach, recognizing that a patient’s needs evolve as they progress through different developmental stages.
Core Principle: Tailoring care to the patient’s age and life stage enhances outcomes and ensures age-appropriate support.
- Example: An elderly patient with arthritis may need modifications in their home to safely perform self-care tasks, while a child recovering from surgery may benefit from playful therapy activities.
- Key Insight: Lifespan-focused care ensures that interventions remain relevant and effective across all age groups.
- Think of it as… Switching gears on a bicycle—adjustments are necessary based on the terrain and pace of the journey.
Applying the Nursing Process through the Roper-Logan-Tierney Model
Step 1: Assessment – Identifying Gaps in ADLs
Nurses perform a comprehensive assessment of the patient’s ability to carry out ADLs, considering both internal and external factors.
- Example: A patient recovering from hip surgery is assessed for mobility challenges, pain management, and environmental safety.
- Key Insight: Early assessment identifies areas requiring immediate intervention, preventing complications.
- Think of it as… Gathering puzzle pieces to see the complete picture of the patient’s health and needs.
Step 2: Diagnosis – Recognizing Deficiencies in ADLs
The assessment findings guide nurses in diagnosing limitations or risks related to the patient’s ADLs.
- Example: A patient diagnosed with impaired mobility after a fall will require interventions aimed at improving physical function and preventing future injuries.
- Key Insight: Accurate diagnosis ensures care plans target underlying problems and achieve meaningful outcomes.
- Think of it as… Identifying the root cause of a mechanical failure before attempting repairs.
Step 3: Planning – Developing ADL-Focused Interventions
A personalized care plan is developed based on the patient’s strengths, limitations, and external influences affecting their ADLs.
- Example: For a patient with difficulty bathing independently, the plan may include installing grab bars, physical therapy, and caregiver assistance.
- Key Insight: Collaborative planning ensures that interventions are practical, achievable, and patient-centered.
- Think of it as… Designing a travel itinerary—each step is planned to meet the destination successfully.
Step 4: Implementation – Executing Care Plans
Nurses put the plan into action by coordinating nursing interventions, physical therapy, and patient education.
- Example: A nurse assists a patient with mobility exercises while teaching them proper techniques to avoid strain and injury.
- Key Insight: Successful implementation requires flexibility and continuous monitoring of patient progress.
- Think of it as… Following a recipe—making adjustments as needed to achieve the best results.
Step 5: Evaluation – Measuring Progress and Adjusting Care Plans
Nurses evaluate whether the patient’s ADLs have improved and adjust the care plan accordingly to address any unmet needs.
- Example: If a patient’s mobility shows minimal progress, additional physical therapy sessions or new assistive devices may be introduced.
- Key Insight: Continuous evaluation ensures that the care plan evolves with the patient’s changing needs.
- Think of it as… Checking the GPS during a road trip—real-time updates help avoid detours and delays.
Practical Applications of the Roper-Logan-Tierney Model in Nursing Practice
I) Enhancing Functional Independence in Acute Care Settings
This model helps nurses support patients in regaining independence during their recovery from surgery or illness.
- Example: A nurse assists a post-operative patient in progressively resuming daily activities like walking and dressing.
- Key Insight: Focusing on functional independence improves patient outcomes and prevents complications.
- Think of it as… Helping someone rebuild their strength step by step after a setback.
II) Chronic Care Management: Maintaining Long-Term Functionality
The model addresses the ongoing needs of patients with chronic conditions, helping them maintain optimal functionality and quality of life.
- Example: A patient with COPD receives home-based care, including breathing exercises and dietary modifications.
- Key Insight: Continuous support and tailored interventions prevent deterioration and enhance long-term outcomes.
- Think of it as… Steering a boat through changing tides—constant adjustment is necessary for smooth sailing.
III) Community-Based Care: Promoting Independence at Home
Nurses apply this model to patients transitioning from hospital to home by ensuring they have access to the resources needed to maintain ADLs.
- Example: A cancer survivor transitioning to home care is connected with support services, such as counseling and nutritional advice.
- Key Insight: Community-based interventions bridge gaps in care and provide patients with essential tools for independent living.
- Think of it as… Building a safety net to support patients after they leave the structured environment of the hospital.
Case Studies Demonstrating the Roper-Logan-Tierney Model of Nursing
Case Study 1: Post-Surgery Rehabilitation for a Hip Replacement Patient
Scenario: A 70-year-old patient undergoes hip replacement surgery and faces challenges with mobility, personal hygiene, and maintaining a safe environment.
Application of the Model:
- Assessment: The nurse evaluates the patient’s ability to walk, dress, and maintain hygiene independently, identifying the need for assistive devices and environmental modifications.
- Diagnosis: Impaired mobility related to post-surgery pain and weakness.
- Planning: The care plan includes physical therapy sessions, adaptive tools for dressing, and grab bars installed at home to reduce fall risk.
- Implementation: Nurses coordinate with physical therapists, educate the patient on using mobility aids, and provide assistance with personal hygiene until independence is restored.
- Evaluation: Weekly assessments show gradual improvement in mobility, and the patient transitions to performing daily tasks with minimal assistance.
Example: The patient progresses from using a walker to a cane within six weeks.
Key Insight: A multidisciplinary approach ensures that both physical and environmental factors are addressed for effective rehabilitation.
Think of it as… Building scaffolding around a building under renovation—each support helps the structure regain its strength.
Case Study 2: Managing Chronic Illness in a COPD Patient
Scenario: A 60-year-old patient with chronic obstructive pulmonary disease (COPD) experiences difficulty breathing and limited mobility, leading to challenges with ADLs such as eating, bathing, and sleeping.
Application of the Model:
- Assessment: The nurse evaluates the patient’s respiratory function, nutrition, and ability to perform daily tasks independently.
- Diagnosis: Impaired breathing and fatigue affecting activities of daily living.
- Planning: The care plan includes breathing exercises, dietary modifications, and sleep hygiene strategies to improve overall function.
- Implementation: Nurses provide oxygen therapy, teach the patient relaxation techniques, and recommend small, frequent meals to maintain energy levels.
- Evaluation: Regular check-ins show improved breathing patterns, better nutrition, and more restful sleep, allowing the patient to resume light household activities.
Example: The patient reports fewer episodes of breathlessness and improved energy levels within three months of the care plan.
Key Insight: Addressing interconnected issues such as breathing, nutrition, and sleep promotes overall well-being.
Think of it as… Tuning a musical instrument—each component must work in harmony for optimal performance.
Case Study 3: Transitioning an Elderly Patient to Home Care
Scenario: An 85-year-old patient is discharged from the hospital after recovering from pneumonia and requires home-based care to regain independence.
Application of the Model:
- Assessment: The nurse evaluates the patient’s ability to manage ADLs, including personal hygiene, mobility, and medication adherence.
- Diagnosis: Risk of falls and self-care deficits related to weakness post-illness.
- Planning: The care plan includes home modifications, caregiver support, and exercises to rebuild strength.
- Implementation: The patient receives daily visits from a home care nurse, exercises to improve muscle strength, and caregiver support for tasks like bathing and meal preparation.
- Evaluation: Over time, the patient regains sufficient strength to resume light household activities independently while maintaining safety precautions.
Example: The patient progresses from requiring assistance for bathing to performing personal hygiene tasks independently.
Key Insight: Coordinating home care with patient education and environmental modifications ensures a smooth transition.
Think of it as… Guiding someone across a bridge—they start with assistance and eventually cross it independently.
Modern Implications of the Roper-Logan-Tierney Model of Nursing
I) Promoting Holistic Patient-Centered Care
The Roper-Logan-Tierney model encourages nurses to assess patients beyond their physical symptoms, incorporating psychological, environmental, and social factors to deliver comprehensive care.
- Example: A nurse working with a cancer patient not only manages pain but also addresses emotional support and social isolation through counseling and community resources.
- Key Insight: Holistic assessments help nurses design interventions that address the full spectrum of patient needs, improving overall well-being.
- Think of it as… Viewing a painting from multiple angles—each perspective reveals details that contribute to the full picture.
II) Enhancing Functional Independence Across Care Settings
The model’s focus on ADLs ensures that nursing interventions are designed to restore or maintain patient independence, whether in acute care, chronic care, or community-based settings.
- Example: A stroke patient initially dependent on caregivers for personal hygiene regains independence through assistive devices and tailored physical therapy.
- Key Insight: Encouraging independence promotes dignity, self-confidence, and faster recovery.
- Think of it as… Teaching someone to ride a bike—they need initial support but eventually take control on their own.
III) Guiding Age-Appropriate Care Through the Lifespan
The lifespan approach embedded in the model ensures that nursing care is tailored to the patient’s developmental stage, whether for children, adults, or the elderly.
- Example: A pediatric patient recovering from surgery benefits from play-based physical therapy, while an elderly patient receives home safety modifications.
- Key Insight: Age-specific interventions improve engagement, compliance, and outcomes.
- Think of it as… Customizing a pair of shoes—each pair fits the wearer’s unique size and needs.
IV) Fostering Interdisciplinary Collaboration
The model highlights the importance of collaboration among nurses, physicians, physical therapists, social workers, and other healthcare professionals to address complex patient needs.
- Example: A patient recovering from a hip replacement benefits from the combined efforts of a nurse, physical therapist, and social worker to ensure physical recovery and home safety.
- Key Insight: Collaborative care enhances the effectiveness of interventions and prevents care gaps.
- Think of it as… Playing in an orchestra—each member contributes to a harmonious performance.
V) Supporting Long-Term Health through Community-Based Programs
The model extends beyond hospital settings to guide community health initiatives that support patients in managing chronic conditions and maintaining ADLs at home.
- Example: A diabetes patient is enrolled in a community program that offers nutrition workshops, exercise classes, and mental health support.
- Key Insight: Community resources bridge the gap between clinical care and everyday living, fostering sustained health improvements.
- Think of it as… Building a network of bridges—each link supports patients as they transition between different care settings and life stages.
Challenges and Limitations of the Roper-Logan-Tierney Model of Nursing
I) Time Constraints in Fast-Paced Clinical Settings
Nurses often face time limitations in acute or emergency care settings, which can make it difficult to perform comprehensive ADL assessments and develop personalized care plans.
- Example: In a busy emergency department, nurses may only have time to assess immediate physical needs, such as breathing and mobility, while overlooking long-term considerations like emotional support or communication.
- Key Insight: Streamlining assessment tools and prioritizing critical ADLs can help nurses efficiently manage patient care even in time-sensitive situations.
- Think of it as… Managing a time-limited cooking show—focusing on essential steps ensures the outcome is still successful despite time constraints.
II) Patient Non-Compliance with Recommended Interventions
Patients may resist following care plans due to fear, lack of understanding, or motivational issues, which can hinder recovery and compromise independence.
- Example: A patient recovering from surgery may skip physical therapy sessions due to pain or frustration, delaying their progress in regaining mobility.
- Key Insight: Providing consistent education, emotional support, and involving patients in the planning process can improve adherence and motivation.
- Think of it as… Watering a plant regularly—ongoing encouragement and care help foster steady growth.
III) Limited Resources and Accessibility in Community Settings
Patients transitioning from hospital to home care or community-based programs may face limited access to necessary resources, such as assistive devices, physical therapy, or home modifications.
- Example: An elderly patient living in a rural area may not have access to home care services or specialized equipment needed for daily activities.
- Key Insight: Collaboration with community organizations and government programs can bridge the resource gap and ensure patients receive the support they need.
- Think of it as… Creating a patchwork quilt—each resource adds a piece to the bigger picture of comprehensive care.
IV) Managing Complex Patients with Multiple Health Conditions
Patients with co-existing chronic illnesses, such as diabetes and heart disease, may present overlapping ADL challenges that require multidimensional and coordinated interventions.
- Example: A diabetic patient recovering from a stroke may need support with both dietary modifications and mobility exercises, requiring collaboration among multiple specialists.
- Key Insight: An interdisciplinary approach ensures that all aspects of the patient’s needs are addressed effectively.
- Think of it as… Solving a multi-piece puzzle—each piece must fit perfectly to complete the picture.
V) Balancing Holistic and Task-Oriented Nursing
While the Roper-Logan-Tierney Model advocates holistic care, task-oriented environments may prioritize physical tasks over psychological or emotional needs due to workload demands.
- Example: A nurse may prioritize tasks like administering medications and monitoring vital signs, leaving little time to assess the patient’s emotional well-being.
- Key Insight: Integrating emotional and social assessments into routine physical care tasks can help balance holistic and task-oriented approaches.
- Think of it as… Stirring two ingredients at once—both physical and emotional assessments can be combined to create a seamless approach to care.
Roper-Logan-Tierney Model of Nursing Quiz
1) What is the primary focus of the Roper-Logan-Tierney Model of Nursing?
a) Standardizing medical procedures
b) Managing patient medications
c) Enhancing independence through the assessment of ADLs
d) Ensuring compliance with doctor’s orders
2) Which ADL involves assessing the patient’s ability to maintain cleanliness and hygiene?
a) Mobilizing
b) Personal cleansing and dressing
c) Communicating
d) Eliminating waste
3) What is an example of promoting functional independence in the Roper-Logan-Tierney Model?
a) Encouraging a patient to rely solely on caregivers
b) Educating a patient on the proper use of mobility aids
c) Providing constant supervision without teaching self-care
d) Limiting the patient’s physical activity for safety
4) Why is interdisciplinary collaboration important when applying the Roper-Logan-Tierney Model?
a) To reduce the number of healthcare providers involved
b) To address overlapping ADL challenges comprehensively
c) To minimize the role of nurses
d) To focus solely on physical rehabilitation
5) What strategy can help manage patient non-compliance with recommended interventions?
a) Reducing communication with the patient
b) Providing consistent education and emotional support
c) Ignoring the patient’s concerns
d) Enforcing mandatory compliance without discussion
Quiz Answers with Rationale
- c) Enhancing independence through the assessment of ADLs
Rationale: The model focuses on assessing and supporting the patient’s ability to perform activities of daily living, promoting autonomy and well-being. - b) Personal cleansing and dressing
Rationale: This ADL involves evaluating and supporting the patient’s ability to maintain hygiene and dress independently. - b) Educating a patient on the proper use of mobility aids
Rationale: Promoting independence involves providing patients with the knowledge and tools to perform tasks with minimal assistance. - b) To address overlapping ADL challenges comprehensively
Rationale: Interdisciplinary collaboration ensures that different aspects of patient needs—physical, emotional, and social—are addressed effectively. - b) Providing consistent education and emotional support
Rationale: Continuous education and emotional support help patients overcome resistance and adhere to care plans, improving outcomes.
Questions and Answers on the Roper-Logan-Tierney Model of Nursing
Q1: What is the main goal of the Roper-Logan-Tierney Model of Nursing?
A: The main goal is to promote patient independence and improve their quality of life by assessing and supporting their ability to perform activities of daily living.
Q2: How does the model help nurses provide holistic care?
A: By focusing on the 12 ADLs, the model ensures that nurses address physical, psychological, social, and environmental factors affecting the patient’s well-being.
Q3: Why is assessment of ADLs critical in nursing care?
A: Assessing ADLs helps identify areas where patients need support, guiding individualized interventions that promote recovery, independence, and long-term well-being.
Q4: What role does interdisciplinary collaboration play in this model?
A: Interdisciplinary collaboration allows healthcare providers from various specialties to work together, ensuring that complex patient needs—such as mobility, nutrition, and emotional support—are comprehensively managed.
Q5: How can nurses address patient non-compliance with care plans?
A: Nurses can provide consistent education, engage the patient in the care planning process, and offer emotional support to improve adherence to interventions and motivate patients toward recovery.
Q5: How can nurses address patient non-compliance with care plans?
A: Nurses can provide consistent education, engage the patient in the care planning process, and offer emotional support to improve adherence to interventions and motivate patients toward recovery.
Q6: When was the Roper-Logan-Tierney Model developed?
A: The model was developed in 1980 by Nancy Roper, Winifred Logan, and Alison Tierney.
It has since evolved through updates to reflect modern nursing needs and practices.
Q7: What are the 12 activities of daily living in the Roper-Logan-Tierney Model?
A: The 12 ADLs include maintaining a safe environment, communication, breathing, eating and drinking, eliminating waste, personal cleansing and dressing, controlling body temperature, mobilizing, working and playing, sleeping, expressing sexuality, and dying.
Conclusion of the Roper-Logan-Tierney Model of Nursing
The Roper-Logan-Tierney Model of Nursing, developed by Nancy Roper, Winifred Logan, and Alison Tierney, focuses on promoting independence by addressing the 12 activities of daily living (ADLs).
Its holistic approach ensures that nurses provide comprehensive care, meeting patients’ physical, emotional, and social needs.
With applications in acute care, chronic illness management, and community settings, the model remains highly adaptable and effective.
Its emphasis on interdisciplinary collaboration and patient-centered care makes it an enduring framework for improving health outcomes.
Final Reflective Question: How can you incorporate this model into your clinical practice to promote patient independence and holistic recovery?