Afaf Meleis is a distinguished nursing theorist, globally recognized for her contributions to nursing education and research.
Her Transitions Theory highlights the role of nurses in supporting individuals as they navigate major life changes, such as illness, recovery, and developmental milestones.
The theory emphasizes the significance of understanding and managing transitions—whether developmental, situational, or health-related—to improve patient outcomes.
It serves as a framework to help nurses guide patients through periods of change while promoting stability and well-being.
This article will explore the core concepts, practical applications, and case studies of Meleis’ Transitions Theory in nursing practice, with a focus on transitional care.
What You’ve Learned – Afaf Meleis’ Transitions Theory
- Holistic approach to transitions: Meleis’ theory emphasizes that life transitions—whether health, developmental, or situational—affect patients physically, emotionally, and socially.
- Individualized, patient-centered care: Nurses play a crucial role in assessing unique transition challenges and tailoring interventions that fit each patient’s needs.
- Interdisciplinary collaboration improves outcomes: Working with healthcare teams ensures that patients receive comprehensive support throughout their transition.
- Ongoing assessment and evaluation: Regular monitoring allows nurses to adjust care plans, ensuring patients progress smoothly through their transition stages.
- Empowering patients enhances self-efficacy: Involving patients in decision-making fosters independence and improves adherence to care plans, leading to better long-term outcomes.
Core Concepts of Afaf Meleis’ Transitions Theory
Afaf Meleis’ Transitions Theory revolves around understanding and managing various transitions that patients undergo.
Nurses play a critical role in assessing these transitions, identifying challenges, and guiding patients toward successful outcomes.
The core concepts include understanding the types of transitions, recognizing patterns of transitions, and identifying key indicators of healthy transitions.
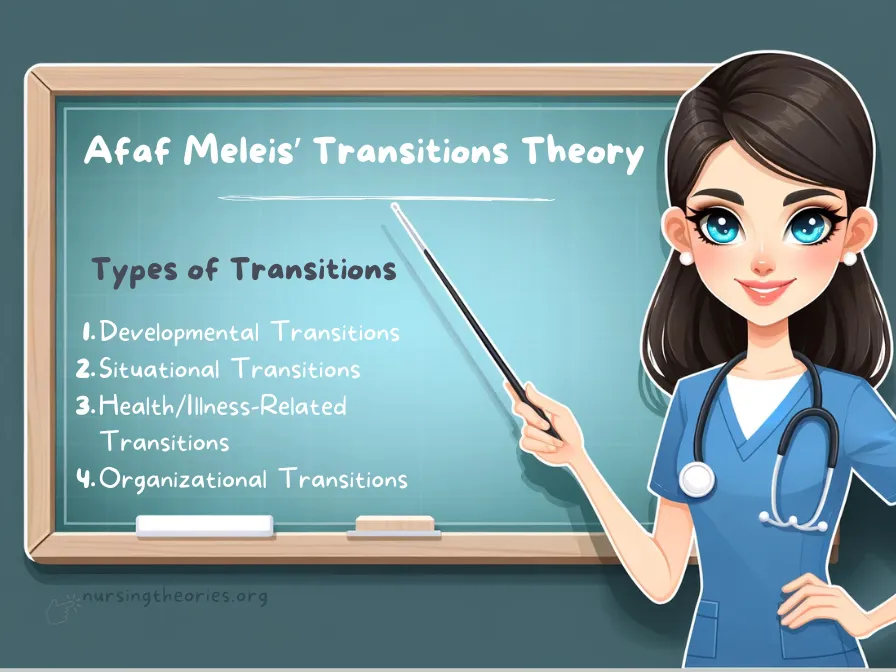
I) Types of Transitions
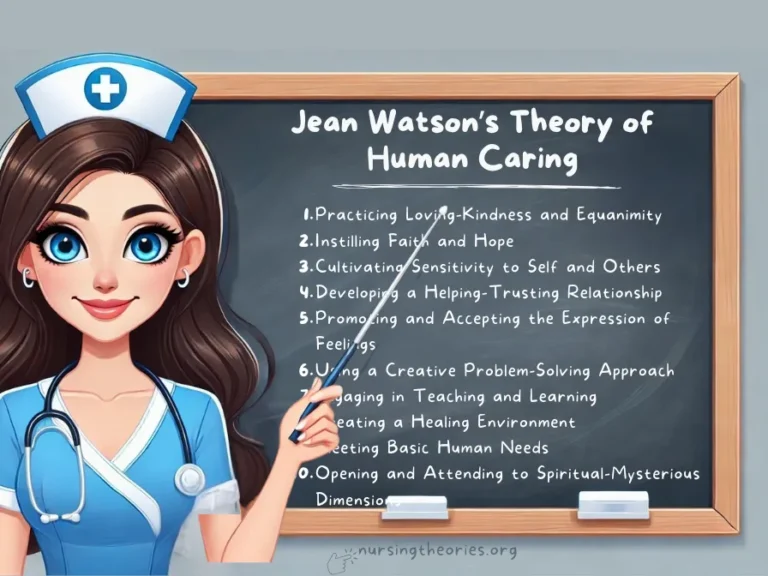
Meleis categorizes transitions into four main types: developmental, situational, health/illness-related, and organizational.
Each type represents a unique life change that may impact a patient’s well-being.
1) Developmental Transitions: These involve changes tied to growth and development across the lifespan, such as puberty, aging, or parenthood.
- Example: An adolescent navigating the emotional and physical changes of puberty.
- Key Insight: Developmental transitions require support to help individuals adapt to new roles and expectations.
- Think of it as… A butterfly emerging from a cocoon—each stage requires adjustment for the next.
2) Situational Transitions: These occur due to changes in life circumstances, such as relocation, job changes, or becoming a caregiver.
- Example: A patient adjusting to life after moving into a long-term care facility.
- Key Insight: Situational transitions often require external support systems to help individuals adapt.
- Think of it as… Moving to a new city where everything is unfamiliar but gradually becomes home.
3) Health/Illness-Related Transitions: These relate to changes in health status, such as diagnosis, recovery, or progression of illness.
- Example: A patient newly diagnosed with diabetes learning to manage their condition.
- Key Insight: Timely education and emotional support are crucial to managing health transitions successfully.
- Think of it as… Learning to drive a car for the first time—new knowledge and practice are key.
4) Organizational Transitions: These involve changes within healthcare systems or organizational structures that affect care delivery.
- Example: A hospital undergoing a shift to electronic health records and training its staff to adapt.
- Key Insight: Successful organizational transitions depend on effective communication and collaboration.
- Think of it as… A team adopting a new playbook—everyone needs to be on the same page for success.
II) Patterns of Transition
Meleis identifies three patterns of transition: single, multiple, and sequential.
Recognizing these patterns helps nurses anticipate potential challenges and develop effective interventions.
1) Single Transitions: These involve one significant change occurring at a time.
- Example: A patient transitioning from hospital care to home recovery.
- Key Insight: Single transitions are easier to manage but still require attention to emotional and physical adjustment.
- Think of it as… Focusing on one road at a time, making navigation straightforward.
2) Multiple Transitions: Involves experiencing several simultaneous changes, such as health, family, or work-related transitions occurring together.
- Example: A patient recovering from surgery while also coping with job loss.
- Key Insight: Multiple transitions can intensify stress, requiring holistic, coordinated care.
- Think of it as… Juggling multiple tasks that demand different types of focus.
3) Sequential Transitions: These occur in a series, where one transition leads into another.
- Example: A patient completes rehabilitation and then begins outpatient therapy for further recovery.
- Key Insight: Sequential transitions require continuous follow-up to ensure smooth progression.
- Think of it as… Following a series of stepping stones to reach the final goal.
III) Indicators of a Healthy Transition
Meleis identifies key indicators that show whether patients are successfully adapting to changes, focusing on emotional stability, effective coping mechanisms, and active patient engagement.
1) Emotional Stability: Maintaining emotional balance and managing stress effectively during transitions.
- Example: A post-operative patient shows no signs of anxiety while adapting to physical therapy.
- Key Insight: Emotional stability supports long-term recovery and successful outcomes.
- Think of it as… Balancing on a tightrope—steady emotions help maintain progress without setbacks.
2) Effective Coping Mechanisms: The ability to develop and implement strategies for dealing with transition-related challenges.
- Example: A patient newly diagnosed with a chronic illness joins a support group and follows lifestyle changes.
- Key Insight: Coping mechanisms ensure resilience and prevent patients from feeling overwhelmed.
- Think of it as… Carrying an umbrella—preparedness for changing weather ensures stability.
3) Active Patient Engagement: The patient’s involvement in decision-making and self-care activities related to their transition.
- Example: A cancer survivor actively participates in follow-up care and monitors their health improvements.
- Key Insight: Engagement empowers patients to take ownership of their recovery and health outcomes.
- Think of it as… Steering a car—the patient is in control of their journey to well-being.
The Nursing Process in Afaf Meleis’ Transitions Theory
Step 1: Assessment – Gathering Comprehensive Information
Nurses gather information about the patient’s current transition, including challenges, coping mechanisms, and support systems.
Example: Assessing a newly diagnosed diabetic patient involves understanding their emotional response, knowledge gaps, and readiness for lifestyle changes.
Key Insight: A thorough assessment enables nurses to design individualized interventions that address both immediate and long-term needs.
Think of it as… Peeling back the layers of an onion to uncover the core challenges affecting the patient’s adaptation.
Step 2: Diagnosis – Identifying Challenges and Goals
Based on the assessment, nurses identify specific challenges and establish individualized goals for the patient’s transition.
Example: A goal may be to help a patient regain confidence in managing their daily insulin injections.
Key Insight: Setting clear and achievable goals ensures that interventions are targeted and progress is measurable.
Think of it as… Plotting checkpoints on a map—each goal is a milestone guiding the patient toward successful adaptation.
Step 3: Planning – Developing an Individualized Care Plan
A personalized care plan is created to address the patient’s unique needs, integrating medical, emotional, and social support.
Example: For a patient recovering from heart surgery, the care plan may include medication management, physical therapy, and emotional counseling.
Key Insight: Collaboration with patients and families ensures that interventions are practical, achievable, and supported in the home environment.
Think of it as… Designing a custom-fit suit—every element of the plan is tailored to fit the patient’s specific needs.
Step 4: Implementation – Providing Care Across All Dimensions
The care plan is put into action through coordinated nursing interventions that address both physical and emotional needs.
Example: A nurse ensures that a post-operative patient receives pain management, emotional support, and follow-up assessments.
Key Insight: Effective implementation requires flexibility and ongoing communication to meet evolving patient needs.
Think of it as… Building a bridge where every step is carefully planned to ensure a safe crossing.
Step 5: Evaluation – Assessing the Effectiveness of Care
Continuous monitoring and evaluation help nurses determine the effectiveness of the transition plan.
Example: A nurse monitors a stroke patient’s progress during rehabilitation, adjusting the plan as needed to accommodate changes in mobility or cognitive function.
Key Insight: Regular evaluation ensures that any issues are identified early and the care plan remains effective.
Think of it as… Checking the GPS during a road trip—making adjustments keeps the journey on track and avoids unnecessary detours.
Practical Applications of Afaf Meleis’ Transitions Theory in Nursing Practice
Afaf Meleis’ Transitions Theory has broad applications in various healthcare settings, where its holistic approach to transitional care supports patients’ physical, emotional, and social well-being.
Nurses can use this framework to guide interventions that help patients adapt to life changes while minimizing adverse outcomes.
I) In Acute Care
Meleis’ theory helps nurses address critical transitions, such as those involving hospital admissions or post-discharge care.
By recognizing patients’ vulnerability during transitions, nurses can create plans to reduce complications.
Example: A patient discharged after surgery is provided with a follow-up care plan involving home visits and telehealth consultations.
Key Insight: Preventing hospital readmissions is achievable by supporting the patient’s physical recovery and addressing psychosocial needs.
Think of it as… Providing a safety net that catches potential problems before they escalate.
II) In Chronic Care
Chronic illness management benefits significantly from Meleis’ framework, as patients often face ongoing transitions related to disease progression or treatment changes.
Example: A patient with heart failure is educated on recognizing early warning signs and given resources for emotional support.
Key Insight: Helping patients adapt continuously to evolving health challenges reduces stress and enhances adherence to long-term treatment plans.
Think of it as… Steering a boat through changing tides—constant navigation ensures the patient stays on course.
III) In Community-Based Care
Transitions within community settings, such as from hospital to home or from one healthcare provider to another, require coordination to ensure continuity of care.
Example: A cancer survivor transitioning from hospital care to home is connected with community resources like counseling services and support groups.
Key Insight: Community support networks bridge gaps in care and provide patients with the tools needed for independent living.
Think of it as… Creating a support bridge—community resources act as the pillars holding the structure together.
Practical Applications of Afaf Meleis’ Transitions Theory in Nursing Practice
I) Practical Applications of Afaf Meleis’ Transitions Theory in Acute Care Settings
Meleis’ theory helps nurses address critical transitions, such as those involving hospital admissions or post-discharge care.
By recognizing patients’ vulnerability during transitions, nurses can create plans to reduce complications.
Example: A patient discharged after surgery is provided with a follow-up care plan involving home visits and telehealth consultations.
Key Insight: Preventing hospital readmissions is achievable by supporting the patient’s physical recovery and addressing psychosocial needs.
Think of it as… Providing a safety net that catches potential problems before they escalate.
II) Practical Applications of Afaf Meleis’ Transitions Theory in Chronic Care Management
Chronic illness management benefits significantly from Meleis’ framework, as patients often face ongoing transitions related to disease progression or treatment changes.
Example: A patient with heart failure is educated on recognizing early warning signs and given resources for emotional support.
Key Insight: Helping patients adapt continuously to evolving health challenges reduces stress and enhances adherence to long-term treatment plans.
Think of it as… Steering a boat through changing tides—constant navigation ensures the patient stays on course.
III) Practical Applications of Afaf Meleis’ Transitions Theory in Community-Based Nursing Care
Transitions within community settings, such as from hospital to home or from one healthcare provider to another, require coordination to ensure continuity of care.
Example: A cancer survivor transitioning from hospital care to home is connected with community resources like counseling services and support groups.
Key Insight: Community support networks bridge gaps in care and provide patients with the tools needed for independent living.
Think of it as… Creating a support bridge—community resources act as the pillars holding the structure together.
Case Studies Demonstrating Afaf Meleis’ Transitions Theory
Case Study 1: Supporting a Patient Transitioning to Long-Term Care
Scenario: A 75-year-old patient with Parkinson’s disease moves from independent living to a long-term care facility due to progressive symptoms.
Application of the Theory: Nurses conducted a thorough assessment of the patient’s emotional and physical challenges, including feelings of isolation and concerns about diminished independence.
An individualized care plan was developed to support both physical therapy and emotional well-being.
Key Insight: Focusing on both physical and psychosocial aspects of transitions ensures holistic adaptation.
Think of it as… Building a strong foundation—addressing both physical and emotional needs helps maintain overall stability.
Case Study 2: Helping a Postpartum Mother Navigate Emotional Transitions
Scenario: A new mother experiencing postpartum depression after the birth of her second child struggles to adapt to her new role.
Application of the Theory: The nursing team assessed her emotional well-being, identified signs of anxiety and fatigue, and implemented a plan involving counseling, peer support, and sleep interventions.
Key Insight: Addressing emotional distress during major life changes promotes faster recovery and enhances maternal-infant bonding.
Think of it as… Providing a life raft during turbulent waters—nurses help keep patients afloat while navigating emotional waves.
Case Study 3: Managing a Cancer Patient’s Transition from Active Treatment to Palliative Care
Scenario: A 60-year-old cancer patient transitions from active chemotherapy to palliative care following treatment failure.
Application of the Theory: Nurses coordinated with the patient, family, and palliative care team to create a comprehensive care plan addressing pain management, emotional support, and end-of-life discussions.
Key Insight: Managing transitions with sensitivity and compassion ensures patients receive dignified and supportive care.
Think of it as… Creating a peaceful pathway—nurses guide patients toward comfort and dignity during end-of-life care.
Modern Implications of Afaf Meleis’ Transitions Theory in Healthcare
I) Promoting Patient Empowerment
Meleis’ theory emphasizes that successful transitions require patient involvement in their care journey.
Nurses encourage patients to participate in decision-making, fostering self-efficacy and confidence.
- Example: A patient managing diabetes is taught to monitor blood sugar levels and adjust dietary habits independently.
- Key Insight: Empowered patients are more likely to engage in self-care and achieve positive health outcomes.
- Think of it as… Handing over the steering wheel—patients take control of their recovery.
II) Enhancing Interdisciplinary Collaboration
Smooth transitions often depend on coordination among healthcare providers.
Meleis’ theory highlights the need for interdisciplinary teams to work together to ensure continuous, comprehensive care.
- Example: A patient transitioning from hospital to home is supported by a team consisting of nurses, social workers, and physical therapists.
- Key Insight: Collaboration among disciplines reduces gaps in care and improves patient satisfaction.
- Think of it as… An orchestra—each professional plays a role in creating a harmonious care experience.
III) Improving Health Outcomes
By addressing physical, emotional, and social factors, Meleis’ framework helps patients adapt better, leading to improved long-term health.
- Example: A cancer patient transitioning to survivorship care benefits from mental health support and follow-up screenings.
- Key Insight: Addressing multiple dimensions of health ensures comprehensive recovery.
- Think of it as… Cultivating a garden—attention to various aspects of care helps patients flourish.
Challenges and Limitations of Afaf Meleis’ Transitions Theory
I) Time Constraints in Clinical Settings
One of the primary challenges in applying Meleis’ theory is time limitations in fast-paced environments, which can hinder comprehensive assessments and individualized care plans.
- Example: Emergency room nurses may not have sufficient time to assess patients’ long-term needs, focusing instead on immediate treatment.
- Key Insight: Streamlining assessment tools can help optimize the application of the theory, even in time-sensitive settings.
- Think of it as… Managing a sprint during a marathon—balancing immediate care with long-term planning.
II) Patient Non-Compliance
Patients may resist adapting to the changes required during transitions, making it challenging to achieve positive outcomes.
- Example: A patient recovering from surgery may neglect physical therapy sessions due to fear of pain or lack of motivation.
- Key Insight: Providing consistent education and emotional support can address resistance and encourage compliance.
- Think of it as… Watering a plant regularly—consistent care ensures steady growth.
III) Complex Patient Needs
Patients experiencing multiple or overlapping transitions—such as dealing with both acute and chronic conditions—require more comprehensive, multidisciplinary interventions.
- Example: An elderly patient with diabetes and heart disease transitioning from hospital to home requires coordination among various specialists, caregivers, and community services.
- Key Insight: Multidimensional care ensures that all aspects of the patient’s condition are managed effectively.
- Think of it as… Managing multiple puzzle pieces—each piece must fit correctly to see the full picture.
Afaf Meleis’ Transitions Theory Quiz
1) What is the primary focus of Afaf Meleis’ Transitions Theory?
a) Medication adherence
b) Managing life transitions and changes
c) Scheduling appointments
d) Hospital discharge planning
2) Which type of transition includes a change in roles, responsibilities, or life status?
a) Health/illness transition
b) Developmental transition
c) Situational transition
d) Organizational transition
3) How does Meleis’ theory contribute to interdisciplinary collaboration?
a) By eliminating the need for collaboration
b) By integrating teams to ensure smooth transitions
c) By standardizing medical procedures
d) By promoting solo decision-making
4) Why is evaluating patient outcomes important in transitional care?
a) To terminate care plans immediately
b) To ensure transitions are effective and meet goals
c) To increase medication dosage
d) To reduce the number of interventions
5) What strategy can help mitigate patient non-compliance during transitions?
a) Providing limited patient education
b) Consistent education and emotional support
c) Ignoring resistance
d) Reducing communication with patients
Afaf Meleis’ Transitions Theory Quiz Answers with Rationale
- b) Managing life transitions and changes
Rationale: Meleis’ theory centers on guiding patients through transitions, including developmental, health-related, and situational changes. - b) Developmental transition
Rationale: Developmental transitions involve life stage changes, such as becoming a parent or entering retirement. - b) By integrating teams to ensure smooth transitions
Rationale: Interdisciplinary collaboration ensures that different aspects of care are coordinated effectively. - b) To ensure transitions are effective and meet goals
Rationale: Evaluating outcomes allows for adjustments to the care plan, ensuring continued progress. - b) Consistent education and emotional support
Rationale: Providing ongoing support addresses resistance and helps patients adhere to care plans.
Questions and Answers on Afaf Meleis’ Transitions Theory
Q1: What is the main goal of Afaf Meleis’ Transitions Theory?
A: The main goal is to help patients navigate life transitions successfully by providing individualized, holistic care.
Q2: How do nurses identify the type of transition a patient is experiencing?
A: Nurses identify the type of transition by assessing life changes, health conditions, or external factors influencing the patient’s situation.
Q3: Why is interdisciplinary collaboration critical in transitional care?
A: Collaboration ensures that all aspects of a patient’s care—physical, emotional, and social—are addressed, leading to better outcomes.
Q4: How can nurses overcome time constraints when applying the theory?
A: Streamlining assessments and using standardized tools can help nurses efficiently address patient needs within limited timeframes.
Q5: What role does patient empowerment play in successful transitions?
A: Empowering patients to participate in their care fosters self-efficacy and improves adherence to care plans, enhancing outcomes.
Conclusion of Afaf Meleis’ Transitions Theory
Afaf Meleis’ Transitions Theory highlights the importance of understanding and supporting patients during critical life changes.
By integrating individualized care, interdisciplinary collaboration, and ongoing evaluation, nurses can help patients adapt successfully and improve their overall well-being.
The theory’s application in various care settings—from acute care to community-based programs—demonstrates its versatility and continued relevance in modern healthcare.
Final Reflective Question: How can you apply Meleis’ Transitions Theory to improve patient care in your specific clinical setting or practice?