Katharine Kolcaba’s Comfort Theory provides a holistic approach to nursing, where patient well-being is achieved through targeted comfort measures.
By addressing physical, emotional, spiritual, and environmental needs, Kolcaba’s theory enhances healing and patient satisfaction.
This framework has become essential in various care settings, from acute care to palliative environments, due to its practical applications and measurable outcomes.
To explore her contributions further, visit Katharine Kolcaba’s profile.
The purpose of this article is to explore the core concepts of Kolcaba’s Comfort Theory and demonstrate how its three comfort states and four contexts apply in nursing practice.
What You’ve Learned – Katharine Kolcaba’s Comfort Theory
- Comfort is a measurable outcome that directly impacts recovery and patient satisfaction.
- Holistic comfort involves addressing physical, emotional, and environmental needs simultaneously.
- Kolcaba’s three types of comfort—relief, ease, and transcendence—promote comprehensive well-being.
- Applying the theory throughout the nursing process leads to personalized care plans and improved outcomes.
- Comfort-focused interventions benefit patients in acute, chronic, and palliative care settings.
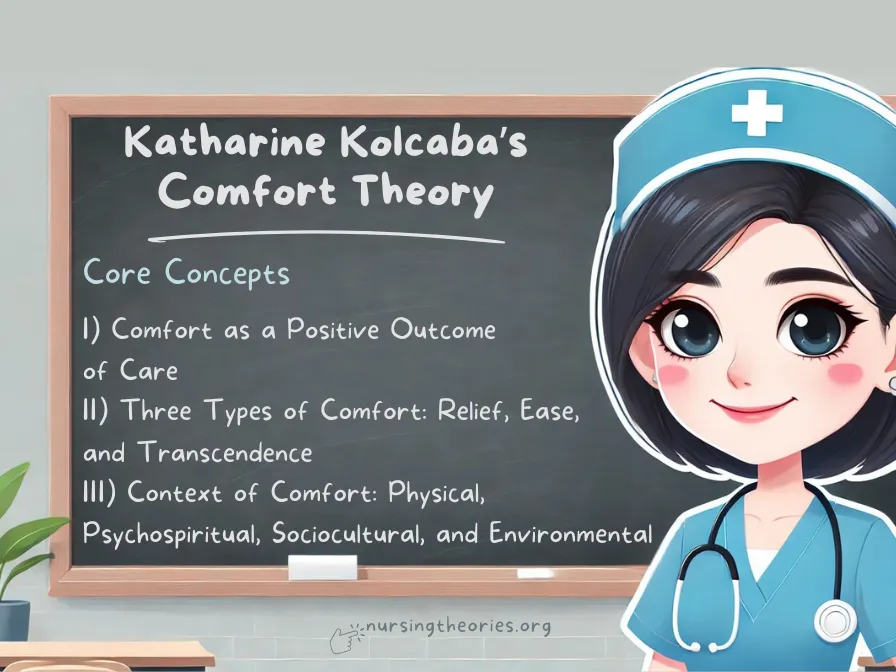
Core Concepts of Katharine Kolcaba’s Comfort Theory
Kolcaba’s Comfort Theory involves three major types of comfort and their contextual applications, making it a comprehensive framework for improving patient care.
I) Comfort as a Positive Outcome of Care
This concept emphasizes that comfort is not just the absence of pain but a holistic state where patients feel physical, emotional, and environmental well-being.
Achieving comfort can enhance healing, emotional balance, and patient satisfaction.
Core Principle: Comfort is a desired and measurable outcome of nursing care that affects healing and well-being.
- Example: A post-operative patient experiences faster recovery due to effective pain management and emotional support.
- Key Insight: When comfort is prioritized, patients are more likely to participate in their recovery actively.
- Think of it as… Creating a warm, supportive environment where healing thrives.
II) Three Types of Comfort: Relief, Ease, and Transcendence
Kolcaba outlines three types of comfort: Relief (immediate alleviation of discomfort), Ease (freedom from discomfort), and Transcendence (rising above challenges to achieve peace).
Together, they encompass physical, emotional, and psychological dimensions of care.
Core Principle: Addressing relief, ease, and transcendence ensures that patients experience comprehensive and lasting comfort.
- Example: Managing a cancer patient’s nausea (relief), providing emotional reassurance (ease), and helping them find purpose through creative outlets (transcendence).
- Key Insight: Addressing all three types of comfort ensures holistic care and long-term well-being.
- Think of it as… A three-legged stool—each component is essential to maintaining balance.
III) Context of Comfort: Physical, Psychospiritual, Sociocultural, and Environmental
Comfort exists within different contexts that nurses must address.
Physical comfort involves pain management, psychospiritual comfort focuses on emotional well-being, sociocultural comfort relates to family and cultural support, and environmental comfort concerns the surrounding space.
Core Principle: Holistic care involves providing comfort across multiple contexts to address the patient’s comprehensive needs.
- Example: A hospital room with soothing lighting, family presence, and supportive conversations enhances a patient’s recovery.
- Key Insight: Addressing comfort across multiple dimensions promotes comprehensive healing.
- Think of it as… Nurturing a plant—physical, emotional, and environmental factors all contribute to growth.
Key Principles of Kolcaba’s Comfort Theory
- Comfort is holistic and measurable
- Patients seek comfort actively
- Enhanced comfort strengthens patients to engage in health-seeking behaviors
- Institutional integrity includes providing comfort care
The Nursing Process Through Katharine Kolcaba’s Comfort Theory
Kolcaba’s Comfort Theory seamlessly integrates with the nursing process, guiding nurses to develop individualized comfort-focused care plans that enhance patient well-being.
By assessing comfort needs and tailoring interventions, nurses can improve patient outcomes across various healthcare settings.
Step 1: Assessment – Identifying Comfort Needs
The assessment phase involves gathering information about the patient’s physical, emotional, and environmental comfort needs.
This includes patient interviews, physical examinations, and observations of non-verbal cues.
Comprehensive assessment is critical to identifying gaps in comfort and creating personalized interventions.
- Example: A nurse assesses a post-surgery patient’s pain levels, emotional state, and environmental conditions, such as noise or room temperature.
- Key Insight: Thorough assessments uncover comfort gaps that may otherwise go unnoticed, allowing for holistic interventions.
- Think of it as… Unpacking a suitcase—each item (or patient need) must be carefully evaluated before organizing a care plan.
Step 2: Diagnosis – Determining Comfort Gaps
Based on the assessment, nurses identify specific comfort deficits that need to be addressed, such as physical pain, emotional distress, or environmental discomfort.
Diagnosing comfort gaps ensures that care plans address targeted needs and focus on restoring balance.
- Example: A cancer patient may be diagnosed with emotional discomfort due to anxiety about treatment, requiring both psychological and physical interventions.
- Key Insight: Pinpointing comfort gaps prevents generalized care and supports tailored interventions.
- Think of it as… Identifying loose puzzle pieces—understanding where they fit is crucial to completing the picture.
Step 3: Planning – Developing a Comfort-Focused Care Plan
The planning phase involves creating a care plan that addresses the identified comfort deficits using relief, ease, and transcendence as guiding principles.
The plan incorporates short-term and long-term interventions.
Effective planning ensures that care interventions are tailored to meet individual comfort needs holistically.
- Example: For a patient with chronic pain, the care plan may include pain management techniques, psychological counseling, and creating a soothing environment.
- Key Insight: Collaborating with the patient during this phase promotes engagement and adherence to the care plan.
- Think of it as… Designing a custom-made outfit—each element is tailored to the patient’s specific needs.
Step 4: Implementation – Delivering Comfort Interventions
The care plan is implemented through nursing interventions that target physical, emotional, and environmental aspects of comfort.
This may involve administering medications, providing emotional support, or making environmental adjustments.
Effective implementation requires flexibility and continuous monitoring to meet evolving comfort needs.
- Example: A nurse caring for a post-operative patient ensures pain relief through medication, emotional support through conversation, and environmental comfort by adjusting room settings.
- Key Insight: Addressing comfort holistically enhances patient satisfaction and accelerates healing.
- Think of it as… Laying down the foundation of a house—every step contributes to a sturdy and supportive structure.
Step 5: Evaluation – Measuring Comfort Outcomes
Continuous evaluation helps nurses assess whether the interventions effectively improve comfort and identify areas that require modification.
Patient feedback, clinical observations, and objective measurements like pain scales are used during this phase.
Ongoing evaluation ensures that care plans remain effective and adapt to changing patient needs.
- Example: A nurse evaluates a palliative care patient’s comfort level through regular check-ins and adjusts pain management strategies as needed.
- Key Insight: Timely evaluations help prevent comfort deficits from escalating and maintain long-term well-being.
- Think of it as… Checking the weather forecast during a road trip—making course corrections ensures the journey stays on track.
Practical Applications of Katharine Kolcaba’s Comfort Theory in Nursing Practice
Kolcaba’s Comfort Theory offers versatile applications across different healthcare settings by providing a holistic framework to promote comfort and improve patient outcomes.
Nurses can integrate the theory into various contexts, including acute, chronic, and palliative care.
I) Enhancing Comfort in Acute Care Settings
In acute care settings, patients often experience short-term pain, anxiety, or discomfort related to surgeries, injuries, or emergency treatments.
By prioritizing immediate comfort needs, nurses can improve recovery times and patient satisfaction.
Core Principle: Providing timely relief through comfort interventions reduces distress and promotes faster recovery.
- Example: A post-operative patient benefits from effective pain management, therapeutic communication, and a calm environment to ease anxiety.
- Key Insight: Addressing both physical and emotional comfort in acute care settings enhances the body’s natural healing processes.
- Think of it as… Cooling a fever—when immediate discomfort is relieved, the body can recover more efficiently.
II) Promoting Comfort in Chronic Illness Management
For patients managing chronic conditions, comfort needs are ongoing and dynamic.
Kolcaba’s theory guides nurses in addressing both persistent symptoms and the psychological challenges associated with long-term conditions.
Core Principle: Maintaining sustained comfort through consistent interventions improves patient adherence and quality of life.
- Example: A patient with rheumatoid arthritis benefits from personalized pain management strategies, emotional support, and ergonomic adaptations in their living environment.
- Key Insight: Continuous evaluation and adaptation of comfort measures prevent symptom exacerbation and improve long-term outcomes.
- Think of it as… Adjusting a sailboat’s direction to navigate changing winds—constant adjustments keep the journey on course.
III) Providing Comfort in Palliative and End-of-Life Care
In palliative care settings, where the primary goal is to ensure quality of life, Kolcaba’s Comfort Theory becomes a central aspect of care.
Nurses address physical pain, emotional distress, and spiritual concerns to provide a peaceful and dignified experience.
Core Principle: Holistic comfort measures during palliative care improve emotional well-being and help patients find meaning and peace.
- Example: A terminally ill patient benefits from pain relief through medication, emotional support through family involvement, and spiritual care from counseling sessions.
- Key Insight: Focusing on comprehensive comfort enables patients to maintain dignity and emotional stability during end-of-life transitions.
- Think of it as… Wrapping a patient in a warm blanket—every layer of care provides additional comfort and protection.
Case Studies Demonstrating Katharine Kolcaba’s Comfort Theory
The following case studies highlight the practical applications of Kolcaba’s Comfort Theory in real-world nursing scenarios, illustrating how comfort interventions lead to improved patient outcomes.
Case Study 1: Managing Pain and Emotional Distress After Surgery
Scenario: A 55-year-old patient underwent major abdominal surgery and experienced significant pain and anxiety postoperatively.
The patient expressed concern about complications and struggled to sleep due to discomfort.
Application of the Theory:
- Assessment: The nurse identified physical pain, emotional distress, and environmental discomfort as key concerns.
- Diagnosis: The patient’s discomfort was attributed to post-surgical pain, fear of complications, and a noisy room environment.
- Intervention: Pain was managed through medication, relaxation techniques reduced anxiety, and environmental adjustments (dim lighting and noise reduction) improved rest.
- Evaluation: The patient reported decreased pain, improved sleep, and reduced anxiety over the next 48 hours.
Key Insight: Holistic comfort interventions can address multiple dimensions simultaneously, leading to faster recovery.
Think of it as… Tuning different instruments in an orchestra—each adjustment creates harmony for healing.
Case Study 2: Supporting Comfort in Long-Term Cancer Treatment
Scenario: A 40-year-old patient undergoing chemotherapy experienced persistent nausea, fatigue, and emotional distress due to fears about the prognosis and side effects.
Application of the Theory:
- Assessment: The nurse assessed physical symptoms like nausea and fatigue, alongside emotional distress related to fear of treatment outcomes.
- Diagnosis: The patient’s comfort deficits included physical discomfort from nausea, psychological distress, and lack of emotional support.
- Intervention: Comfort measures included antiemetic medications, nutritional counseling, psychological counseling, and connecting the patient to a cancer support group.
- Evaluation: The patient experienced fewer episodes of nausea, improved energy, and emotional relief from group participation.
Key Insight: Comprehensive comfort care in chronic conditions helps patients maintain emotional resilience and physical well-being.
Think of it as… Watering different sections of a garden—each area needs attention to thrive.
Case Study 3: Comfort Care in a Palliative Setting
Scenario: A 75-year-old patient with advanced heart failure was admitted to a hospice facility, experiencing chronic pain, difficulty breathing, and existential distress about end-of-life issues.
Application of the Theory:
- Assessment: The nurse identified physical pain, breathlessness, and emotional and spiritual distress as the primary comfort gaps.
- Diagnosis: The patient needed physical relief from pain and breathlessness, as well as spiritual support to cope with end-of-life concerns.
- Intervention: Comfort-focused care included pain management through medication, oxygen therapy, guided relaxation exercises, and spiritual counseling.
- Evaluation: The patient experienced improved pain control, reduced anxiety, and greater emotional peace.
Key Insight: Addressing comfort comprehensively ensures patients receive dignified and compassionate care during end-of-life transitions.
Think of it as… Providing a peaceful pathway where every step brings calm and meaning.
Modern Implications of Katharine Kolcaba’s Comfort Theory in Healthcare
As patient-centered care becomes a priority in modern healthcare, Kolcaba’s Comfort Theory remains highly relevant.
Its holistic approach to well-being has applications in enhancing patient satisfaction, reducing hospital readmissions, and promoting interdisciplinary collaboration.
I) Improving Patient Satisfaction through Comfort Care
Incorporating comfort-focused interventions leads to greater patient satisfaction, as their needs are met beyond clinical treatment.
When patients feel understood and cared for holistically, they are more likely to trust healthcare providers and participate in their recovery.
Core Principle: Satisfied patients are engaged, cooperative, and more likely to experience positive outcomes.
- Example: A post-surgical patient who receives comprehensive comfort care reports higher satisfaction due to reduced pain, emotional reassurance, and a supportive environment.
- Key Insight: Addressing comfort improves the overall patient experience and fosters positive relationships with healthcare providers.
- Think of it as… Providing a full-service experience—when all needs are met, satisfaction naturally follows.
II) Reducing Hospital Readmissions by Meeting Comfort Needs
Addressing comfort deficits during and after hospital stays can prevent complications that lead to readmissions.
Patients who receive effective pain management, emotional support, and post-discharge planning are better equipped to recover independently.
Core Principle: Holistic comfort care reduces risks of setbacks by ensuring patients transition smoothly from hospital to home.
- Example: A patient recovering from heart surgery is less likely to be readmitted due to complications when their physical, emotional, and environmental needs are managed comprehensively.
- Key Insight: Focusing on comfort during transitions promotes recovery and reduces healthcare costs associated with readmissions.
- Think of it as… Building a strong bridge—the better it’s constructed, the less likely anyone is to fall.
III) Enhancing Holistic Nursing Practices through Interdisciplinary Collaboration
Kolcaba’s Comfort Theory promotes collaboration among healthcare teams to meet the various dimensions of comfort.
Nurses, physical therapists, social workers, and counselors work together to provide holistic care, enhancing patient outcomes.
Core Principle: Interdisciplinary collaboration ensures that patients receive comprehensive support from different perspectives.
- Example: A cancer patient benefits from the combined efforts of nurses, dietitians, and psychologists to manage physical symptoms, provide nutritional advice, and offer emotional support.
- Key Insight: Collaborative care results in well-rounded interventions that address all facets of comfort.
- Think of it as… A team sport—every player contributes to the win by working together.
Modern Implications of Katharine Kolcaba’s Comfort Theory in Healthcare
As patient-centered care becomes a priority in modern healthcare, Kolcaba’s Comfort Theory remains highly relevant.
Its holistic approach to well-being has applications in enhancing patient satisfaction, reducing hospital readmissions, and promoting interdisciplinary collaboration.
I) Improving Patient Satisfaction through Comfort Care
Incorporating comfort-focused interventions leads to greater patient satisfaction, as their needs are met beyond clinical treatment.
When patients feel understood and cared for holistically, they are more likely to trust healthcare providers and participate in their recovery.
Core Principle: Satisfied patients are engaged, cooperative, and more likely to experience positive outcomes.
- Example: A post-surgical patient who receives comprehensive comfort care reports higher satisfaction due to reduced pain, emotional reassurance, and a supportive environment.
- Key Insight: Addressing comfort improves the overall patient experience and fosters positive relationships with healthcare providers.
- Think of it as… Providing a full-service experience—when all needs are met, satisfaction naturally follows.
II) Reducing Hospital Readmissions by Meeting Comfort Needs
Addressing comfort deficits during and after hospital stays can prevent complications that lead to readmissions.
Patients who receive effective pain management, emotional support, and post-discharge planning are better equipped to recover independently.
Core Principle: Holistic comfort care reduces risks of setbacks by ensuring patients transition smoothly from hospital to home.
- Example: A patient recovering from heart surgery is less likely to be readmitted due to complications when their physical, emotional, and environmental needs are managed comprehensively.
- Key Insight: Focusing on comfort during transitions promotes recovery and reduces healthcare costs associated with readmissions.
- Think of it as… Building a strong bridge—the better it’s constructed, the less likely anyone is to fall.
III) Enhancing Holistic Nursing Practices through Interdisciplinary Collaboration
Kolcaba’s Comfort Theory promotes collaboration among healthcare teams to meet the various dimensions of comfort.
Nurses, physical therapists, social workers, and counselors work together to provide holistic care, enhancing patient outcomes.
Core Principle: Interdisciplinary collaboration ensures that patients receive comprehensive support from different perspectives.
- Example: A cancer patient benefits from the combined efforts of nurses, dietitians, and psychologists to manage physical symptoms, provide nutritional advice, and offer emotional support.
- Key Insight: Collaborative care results in well-rounded interventions that address all facets of comfort.
- Think of it as… A team sport—every player contributes to the win by working together.
Katharine Kolcaba’s Comfort Theory Quiz
1) What is the primary focus of Katharine Kolcaba’s Comfort Theory?
a) Reducing hospital stay durations
b) Addressing pain through medications
c) Enhancing holistic patient well-being through comfort
d) Standardizing clinical tasks
2) Which of the following best describes Kolcaba’s three types of comfort?
a) Physical, cognitive, and environmental
b) Immediate relief, sustainable recovery, and medication adherence
c) Relief, ease, and transcendence
d) Short-term, mid-term, and long-term comfort
3) What role does interdisciplinary collaboration play in implementing Kolcaba’s Comfort Theory?
a) Reducing the workload of nurses
b) Providing holistic care through diverse professional expertise
c) Standardizing patient satisfaction surveys
d) Limiting patient interaction to clinical tasks
4) How does addressing comfort gaps improve patient outcomes in chronic care?
a) By focusing solely on physical symptoms
b) By promoting active patient engagement and long-term adherence to treatment
c) By shortening treatment durations
d) By standardizing comfort interventions without patient feedback
5) What strategy can help overcome patient resistance to comfort interventions?
a) Limiting communication with the patient
b) Providing continuous education and emotional support
c) Implementing interventions without patient consent
d) Focusing only on immediate medical treatments
Katharine Kolcaba’s Comfort Theory Quiz Answers with Rationale
- c) Enhancing holistic patient well-being through comfort
Rationale: Kolcaba’s theory focuses on addressing physical, emotional, spiritual, and environmental aspects of comfort to improve patient outcomes. - c) Relief, ease, and transcendence
Rationale: Kolcaba’s three types of comfort work together to provide comprehensive care by alleviating immediate pain, reducing distress, and fostering personal growth. - b) Providing holistic care through diverse professional expertise
Rationale: Interdisciplinary collaboration ensures that multiple aspects of a patient’s comfort are addressed through coordinated efforts. - b) By promoting active patient engagement and long-term adherence to treatment
Rationale: Comfort-focused interventions enhance patients’ emotional well-being and motivate them to participate actively in their care, improving outcomes in chronic settings. - b) Providing continuous education and emotional support
Rationale: Educating patients and offering emotional reassurance helps them overcome resistance and engage fully in comfort interventions.
Questions and Answers on Katharine Kolcaba’s Comfort Theory
Q1: What is the core idea behind Kolcaba’s Comfort Theory?
A: The theory focuses on holistic well-being by addressing physical, emotional, and environmental comfort to enhance healing and patient satisfaction.
Q2: How does Kolcaba’s theory apply to end-of-life care?
A: Comfort interventions in palliative settings prioritize pain relief, emotional support, and spiritual care to ensure dignity and quality of life.
Q3: What role does patient feedback play in implementing comfort care?
A: Gathering feedback helps nurses tailor comfort interventions to individual needs and assess the effectiveness of care.
Q4: How can nurses address time constraints when applying Kolcaba’s theory in fast-paced environments?
A: Using streamlined assessment tools and integrating comfort assessments into standard procedures can help optimize care delivery.
Q5: Why is collaboration important when addressing comfort in chronic care?
A: Interdisciplinary collaboration ensures that physical, emotional, and social dimensions of comfort are addressed comprehensively.
Conclusion of Katharine Kolcaba’s Comfort Theory
Katharine Kolcaba’s Comfort Theory provides a comprehensive framework for enhancing patient well-being across diverse healthcare settings.
By addressing physical, emotional, and environmental comfort, nurses can improve recovery, patient satisfaction, and quality of life.
The theory’s emphasis on holistic care, patient-centered interventions, and interdisciplinary collaboration makes it a vital component of modern nursing practice.
Final Reflective Question: How can you apply Kolcaba’s Comfort Theory to create personalized care plans and improve comfort in your specific clinical practice?