Dorothy Johnson’s Behavioral System Model revolutionized nursing by emphasizing the importance of patient behavior and balance in achieving optimal health.
As a nurse and educator, Johnson developed this model to address how disturbances in behavioral systems affect physical and mental well-being.
Learn more about Johnson’s work and impact here.
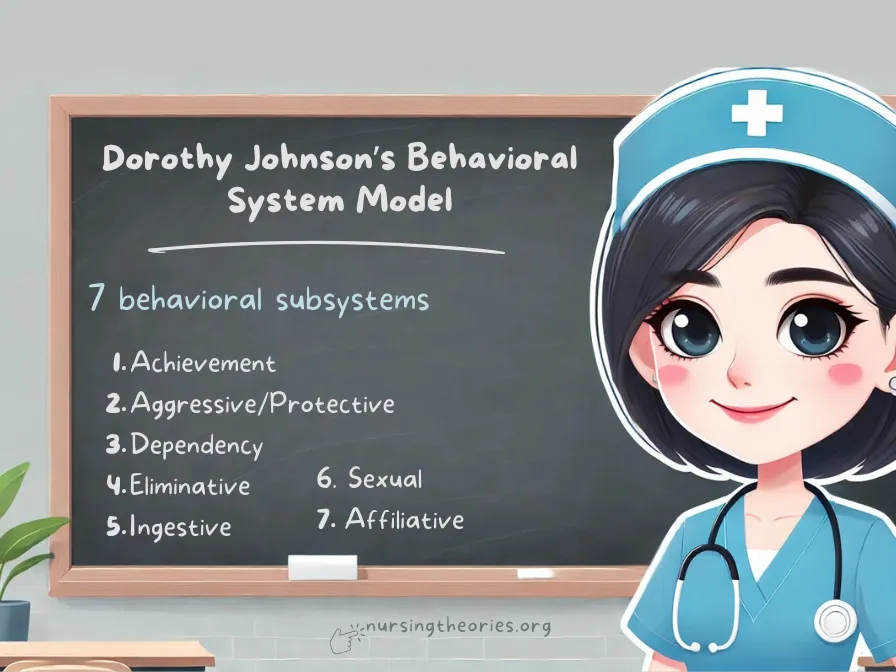
Her model views the patient as a system of seven interrelated subsystems—each with a distinct function—that interact to maintain balance and stability.
This article explores how Johnson’s theory applies to holistic nursing care and its practical uses in various healthcare settings.
What You’ve Learned – Dorothy Johnson’s Behavioral System Model
- Johnson’s model views the patient as a system of seven behavioral subsystems, each playing a crucial role in maintaining overall balance and stability.
- Behavioral disruptions can be caused by both internal (illness, emotions) and external (environment, relationships) stressors, requiring holistic interventions.
- Nurses assess behavioral imbalances, create personalized care plans, and collaborate with interdisciplinary teams to restore stability.
- Continuous assessment and evaluation ensure that care plans are flexible and adapt to the patient’s evolving needs.
- The model is highly applicable in today’s healthcare settings, supporting holistic, behavioral-focused care that integrates both physical and emotional dimensions.
Core Concepts of Dorothy Johnson’s Behavioral System Model
Behavioral Subsystems and Their Roles
Johnson identified seven behavioral subsystems that regulate patient behavior:
- Achievement Subsystem: Focuses on mastery and competence.
- Aggressive/Protective Subsystem: Deals with self-protection and defense mechanisms.
- Dependency Subsystem: Involves seeking nurturing and support.
- Eliminative Subsystem: Regulates waste elimination for physiological health.
- Ingestive Subsystem: Manages food and fluid intake to meet nutritional needs.
- Sexual Subsystem: Relates to sexual identity and procreation.
- Affiliative Subsystem: Involves social bonding and relationships.
Example: A patient recovering from surgery may experience a disruption in the dependency subsystem if they feel isolated or unsupported by family.
Key Insight: Understanding the interaction of these subsystems allows nurses to identify and address specific areas of imbalance, contributing to holistic patient care.
Think of it as… A network of gears in a machine—if one gear stops functioning, the entire system may be affected.
The Concept of Balance and Stability
The goal of Johnson’s model is to maintain or restore behavioral balance.
When one subsystem is disrupted, it affects the patient’s overall health.
Nurses assess these imbalances and design interventions to restore stability.
Example: A patient with anxiety may experience disruptions in both the aggressive/protective subsystem (hypervigilance) and the affiliative subsystem (withdrawal from social interactions).
Key Insight: Maintaining behavioral stability is essential for promoting physical and emotional recovery.
Think of it as… Keeping a tightrope walker balanced—small shifts need immediate correction to prevent a fall.
External and Internal Influences on Behavior
Patient behavior is influenced by internal factors (such as illness or emotions) and external factors (such as the environment or social support).
Nurses must consider both when planning interventions.
Example: A patient experiencing grief may have an imbalance in their affiliative and dependency subsystems, requiring both emotional counseling and support from family.
Key Insight: Effective nursing interventions address not only the patient’s internal state but also their external environment to restore balance.
Think of it as… Tuning an instrument—both internal strings and external settings need to be adjusted for harmony.
Applying Johnson’s Behavioral System Model in Nursing Practice
Step 1: Assessing Behavioral Subsystems
Nurses begin by assessing the patient’s physical, emotional, and behavioral status, identifying which subsystems are imbalanced.
Example: A nurse assesses a patient’s dependency subsystem after a stroke by evaluating their reliance on caregivers for basic tasks.
Key Insight: Thorough assessments provide a clear understanding of behavioral disturbances and their impact on the patient’s overall health.
Think of it as… Creating a map before a journey—you need to know the starting point to plan the best route.
Step 2: Identifying External and Internal Disruptions
Nurses identify stressors that contribute to behavioral instability and determine whether they are internal or external.
Example: A patient’s ingestive subsystem may be disrupted by internal stress (anxiety) or external factors (poor hospital food).
Key Insight: Recognizing the source of the disruption allows for targeted interventions that address the root cause.
Think of it as… Finding the leak before fixing a dripping faucet—you need to solve the underlying issue.
Step 3: Creating a Holistic Care Plan
Nurses collaborate with patients to develop personalized care plans that address behavioral imbalances and promote stability.
Example: For a patient experiencing aggressive behavior due to anxiety, the nurse develops a plan involving cognitive behavioral therapy and stress-relieving activities.
Key Insight: Holistic care plans integrate behavioral, physical, and emotional interventions to ensure comprehensive treatment.
Think of it as… Designing a balanced meal—each component contributes to overall nourishment.
Step 4: Implementing Nursing Interventions to Stabilize Behavior
Nurses implement interventions that directly target the affected subsystems and involve collaboration with other healthcare professionals when necessary.
Example: A nurse administers relaxation techniques and coordinates with a dietitian for a patient with ingestive subsystem imbalances.
Key Insight: Effective implementation requires flexibility, as interventions may need adjustments based on patient response.
Think of it as… Adjusting the sails of a boat—adapt to the wind direction to stay on course.
Step 5: Monitoring and Reassessing Behavioral Stability
Continuous monitoring ensures that interventions are effective, and adjustments are made as needed to maintain long-term stability.
Example: A nurse evaluates a patient’s dependency level weekly after introducing self-care exercises.
Key Insight: Regular reassessments help identify progress and prevent future disruptions.
Think of it as… Checking a compass during a journey—small corrections ensure you reach your destination.
The Nursing Process in Johnson’s Behavioral System Model
Step 1: Holistic Assessment
The first step involves gathering comprehensive data on the patient’s physical, psychological, and behavioral status.
Nurses assess each subsystem to identify any imbalances.
Example: A nurse observes a patient’s lack of appetite and disengagement in social activities, suggesting issues in the ingestive and affiliative subsystems.
Key Insight: Holistic assessments ensure that nurses can identify interconnected problems affecting the patient’s overall well-being.
Think of it as… Performing a full-body check-up before prescribing treatment—you need a complete picture to address the root issue.
Step 2: Diagnosis of Behavioral Imbalances
In this step, nurses identify specific behavioral imbalances within the subsystems and determine their impact on the patient’s health.
Example: The nurse diagnoses social withdrawal as a disruption in the affiliative subsystem, caused by the patient’s feelings of isolation after surgery.
Key Insight: Accurate diagnosis allows nurses to prioritize interventions that address the most pressing issues.
Think of it as… Diagnosing a car issue before repairs—you fix the underlying cause, not just the symptoms.
Step 3: Collaborative Care Planning
Nurses collaborate with patients to create personalized care plans that address identified imbalances while considering the patient’s preferences and goals.
Example: For a patient struggling with dependency, the care plan includes physical therapy and social engagement activities.
Key Insight: Collaborative planning ensures that interventions align with the patient’s values and enhance their involvement in recovery.
Think of it as… Designing a custom-fit suit—it should fit the individual’s unique needs perfectly.
Step 4: Intervention Implementation
This step involves executing the care plan by delivering specific interventions aimed at stabilizing the behavioral subsystems.
Nurses also collaborate with other healthcare professionals as needed.
Example: A nurse works with a social worker to connect a patient to support groups and community resources, stabilizing their affiliative subsystem.
Key Insight: Successful implementation depends on teamwork, flexibility, and the ability to adjust interventions based on patient response.
Think of it as… Following a recipe but tweaking the seasoning based on taste—you adjust to meet the desired outcome.
Step 5: Continuous Evaluation and Adjustment
Nurses continuously monitor the patient’s progress and adjust the care plan if the desired outcomes are not achieved.
This step is crucial for long-term stability.
Example: After monitoring a patient’s progress, the nurse increases the frequency of physical therapy sessions to further improve mobility and reduce dependency.
Key Insight: Ongoing evaluation ensures that care remains effective and responsive to the patient’s changing needs.
Think of it as… Checking your GPS during a road trip—you may need to reroute for optimal results.
Case Studies Using Johnson’s Behavioral System Model
Case Study 1: Managing Dependency Behavior in Post-Surgical Recovery
Scenario: A 70-year-old patient is recovering from hip replacement surgery and exhibits high dependency, relying on nursing staff for assistance with basic tasks like eating, bathing, and moving.
The patient also expresses frustration with their lack of independence.
Application of Johnson’s Behavioral System Model:
- Assessment: The nurse evaluates the patient’s physical, emotional, and behavioral status, noting the dependency on caregivers and low self-efficacy.
- Diagnosis: Disruption in the dependency subsystem is diagnosed, driven by a combination of physical limitations and emotional distress.
- Intervention: The nurse develops a progressive care plan involving physical therapy, gradual self-care activities, and positive reinforcement to boost confidence.
- Evaluation: Over the course of several weeks, the patient demonstrates improved mobility, completing tasks like dressing independently. The nurse adjusts the care plan to introduce more advanced exercises.
- Key Insight: Gradual self-care reintroduction promotes independence, which positively affects both physical and emotional recovery.
- Think of it as… Teaching a person to swim by gradually removing support—confidence builds through small successes.
Case Study 2: Addressing Aggressive Behavior in a Pediatric Patient
Scenario: A 10-year-old child admitted for fracture treatment shows frequent aggressive outbursts, yelling at staff and refusing to cooperate during medical procedures.
Application of Johnson’s Behavioral System Model:
- Assessment: The nurse observes the child’s defensive body language, frustration, and tearful responses when approached by caregivers.
- Diagnosis: The nurse diagnoses an imbalance in the aggressive/protective subsystem, triggered by fear and physical discomfort.
- Intervention: The nurse implements a care plan that includes calming techniques such as storytelling, therapeutic play, and breathing exercises. Parents are encouraged to be present to comfort the child.
- Evaluation: The child’s aggressive responses decrease over time, and cooperation during procedures improves. The nurse monitors progress and adjusts the care plan as needed.
- Key Insight: Addressing emotional triggers with calming interventions can reduce defensive behavior and enhance cooperation.
- Think of it as… Soothing a frightened animal—understanding the fear helps in calming the response.
Case Study 3: Improving Affiliative Behavior in an Isolated Elderly Patient
Scenario: An 85-year-old patient with limited mobility, admitted for chronic heart failure, shows signs of social withdrawal and sadness due to a lack of family visits and community interactions.
Application of Johnson’s Behavioral System Model:
- Assessment: The nurse evaluates the patient’s emotional state, noting withdrawal, decreased appetite, and minimal engagement with staff.
- Diagnosis: Disruption in the affiliative subsystem is identified, linked to isolation and a lack of social interaction.
- Intervention: The nurse introduces the patient to group therapy sessions, schedules virtual family meetings, and engages the patient in community-based activities like music therapy.
- Evaluation: Over time, the patient shows improved mood and engagement during social activities. The nurse evaluates the patient’s progress and suggests expanding their social activities further.
- Key Insight: Strengthening social connections significantly enhances emotional well-being and prevents further isolation.
- Think of it as… Rekindling a fading flame—social interactions fuel emotional recovery and resilience.
Modern Implications of Johnson’s Model in Healthcare
Promoting Holistic and Behavioral-Focused Care
Johnson’s model remains relevant today as it integrates the physical, emotional, and behavioral aspects of health, making it an essential tool in holistic nursing practice.
By addressing the patient as a whole system, nurses can create care plans that address interconnected health challenges.
Example: A patient recovering from cardiac surgery receives physical rehabilitation while nurses address emotional needs through psychological support, preventing relapse.
Key Insight: Holistic care improves patient outcomes by tackling both medical symptoms and underlying emotional or behavioral issues.
Think of it as… Fixing the entire engine of a car instead of patching a leak—comprehensive care leads to sustainable recovery.
Supporting Mental Health Initiatives
With growing awareness of mental health’s role in overall well-being, Johnson’s model provides a framework for understanding behavioral and psychological imbalances.
It allows nurses to assess stress, anxiety, and behavioral changes that impact physical recovery.
Example: A patient with chronic pain may experience disruptions in their dependency and affiliative subsystems, requiring both physical treatment and emotional support to manage pain effectively.
Key Insight: Behavioral assessments ensure that mental health needs are addressed alongside physical ailments.
Think of it as… Watering the roots of a plant, not just the leaves—mental and physical health are interconnected and require joint care.
Encouraging Interdisciplinary Collaboration
Johnson’s model highlights the importance of collaboration between nurses, physicians, social workers, and mental health professionals to restore behavioral stability.
Each professional addresses specific subsystems within the overall care plan.
Example: For a patient recovering from trauma, a team comprising a nurse, a psychologist, and a physical therapist collaborate to address emotional, social, and physical recovery.
Key Insight: Team-based care ensures that each aspect of a patient’s health is covered, minimizing gaps in treatment.
Think of it as… An orchestra working in harmony—each instrument (healthcare professional) contributes to the overall performance (patient recovery).
Challenges and Limitations of Applying Johnson’s Model
Complexity of Behavioral Assessments
One of the key challenges nurses face is conducting comprehensive assessments for all seven subsystems, particularly in fast-paced environments where time is limited.
Example: In emergency settings, nurses may prioritize physical assessments over behavioral ones, potentially overlooking emotional imbalances.
Key Insight: Effective time management and prioritization of critical subsystems can help overcome this limitation.
Think of it as… Deciding which parts of a puzzle to solve first—focus on essential areas before expanding the assessment.
Limited Training in Behavioral Interventions
Not all nurses receive extensive training in behavioral-focused care, making it difficult to apply the model effectively.
Without proper knowledge, interventions may not fully address the root of behavioral disturbances.
Example: A nurse unfamiliar with cognitive behavioral techniques may struggle to help a patient exhibiting signs of aggressive behavior.
Key Insight: Providing continuous professional development and training ensures nurses can apply behavioral interventions confidently.
Think of it as… Learning how to drive before using a car—knowledge is essential for successful implementation.
Handling Complex Patient Needs
Patients with multiple chronic conditions may present imbalances across several behavioral subsystems, making it challenging to prioritize and manage interventions.
Example: A diabetic patient with depression may have imbalances in both the ingestive and affiliative subsystems, requiring coordinated interventions.
Key Insight: Interdisciplinary collaboration and individualized care plans can help manage complex cases effectively.
Think of it as… Untangling a web—addressing one thread at a time helps resolve the entire issue.
Dorothy Johnson’s Behavioral System Model Quiz
1) What is the primary focus of Dorothy Johnson’s Behavioral System Model?
a) Managing physical symptoms only
b) Understanding and stabilizing behavioral subsystems
c) Reducing hospital stays through faster treatment
d) Providing medication-based interventions
2) Which of the following is an example of a disruption in the dependency subsystem?
a) A patient refusing social interaction
b) A patient overly reliant on caregivers for daily tasks
c) A patient experiencing chronic pain
d) A patient following a poor diet
3) What role do external and internal stressors play in Johnson’s model?
a) They have minimal impact on health outcomes
b) They affect only the ingestive subsystem
c) They can cause imbalances across multiple behavioral subsystems
d) They are considered secondary to physical ailments
4)How does Johnson’s model promote interdisciplinary collaboration?
a) By focusing solely on nurse-led care
b) By integrating the efforts of healthcare teams to address holistic patient needs
c) By emphasizing medication-based treatment
d) By limiting care to specific subsystems
5) What is a common challenge nurses face when applying Johnson’s Behavioral System Model?
a) Limited understanding of physical conditions
b) Managing disruptions in only one behavioral subsystem
c) Conducting comprehensive assessments within time constraints
d) Treating only behavioral issues without medical intervention
Dorothy Johnson’s Behavioral System Model Quiz Answers with Rationale
- Correct Answer: b) Understanding and stabilizing behavioral subsystems
Rationale: The core focus of Johnson’s model is to assess and stabilize patient behavior across seven interrelated subsystems to promote overall well-being. - Correct Answer: b) A patient overly reliant on caregivers for daily tasks
Rationale: The dependency subsystem involves seeking nurturing and support, and an imbalance can result in excessive reliance on caregivers. - Correct Answer: c) They can cause imbalances across multiple behavioral subsystems
Rationale: Internal stressors (like anxiety) and external factors (like social isolation) can affect multiple subsystems, leading to imbalances that require holistic intervention. - Correct Answer: b) By integrating the efforts of healthcare teams to address holistic patient needs
Rationale: Johnson’s model encourages interdisciplinary collaboration, allowing various healthcare professionals to address the physical, emotional, and social dimensions of health. - Correct Answer: c) Conducting comprehensive assessments within time constraints
Rationale: One of the challenges of applying Johnson’s model in practice is the time required to conduct detailed behavioral assessments, especially in fast-paced clinical environments.
Questions and Answers on Johnson’s Behavioral System Model
Q1: How do nurses assess behavioral imbalances in Johnson’s model?
A: Nurses assess through observations, interviews, and monitoring patient behaviors related to the seven subsystems to identify disturbances.
Q2: Why is balance important in the behavioral subsystems?
A: Maintaining balance prevents disruptions that could negatively impact a patient’s physical, emotional, and social health.
Q3: How does Johnson’s model support mental health initiatives?
A: By identifying disruptions in behavioral subsystems such as the affiliative or dependency subsystems, nurses can address underlying emotional and psychological issues.
Q4: What is a key strategy for overcoming time-related challenges in assessing patients?
A: Prioritizing subsystems based on the patient’s immediate needs and integrating behavioral assessments into routine care can help manage time effectively.
Q5: How can interdisciplinary collaboration improve outcomes using Johnson’s model?
A: Collaboration ensures that all aspects of a patient’s well-being are addressed by leveraging the expertise of various professionals, from dietitians to mental health specialists.
Conclusion of Dorothy Johnson’s Behavioral System Model
Dorothy Johnson’s Behavioral System Model provides a structured framework for understanding the dynamic relationship between patient behavior and health outcomes.
By focusing on maintaining balance within the seven subsystems, the model ensures that no aspect of a patient’s well-being—whether physical, emotional, or social—is overlooked.
Through effective assessment, personalized care planning, and interdisciplinary collaboration, nurses can deliver holistic care tailored to the individual needs of their patients.
Final Reflective Question: How can nurses effectively integrate behavioral assessments into daily clinical routines to ensure comprehensive and holistic patient care while managing time constraints?