Ida Jean Orlando, a distinguished nursing theorist, revolutionized the nursing profession with her emphasis on dynamic nurse-patient interaction.
Her Deliberative Nursing Process Theory focuses on identifying and meeting immediate patient needs through continuous assessment and problem-solving.
Unlike rigid, pre-planned interventions, Orlando’s model is flexible and responsive, allowing nurses to tailor their care based on real-time cues from patients.
Read Ida Jean Orlando’s biography to learn more about her contributions.
This article explores Orlando’s nursing theory with practical examples and case studies, illustrating how her framework enhances decision-making, promotes patient-centered care, and ensures holistic treatment outcomes.
What You’ve Learned – Ida Jean Orlando’s Deliberative Nursing Process Theory
- Dynamic Nurse-Patient Interaction: At the heart of Orlando’s theory is continuous interaction that enables nurses to identify and address real-time patient needs, fostering personalized care.
- Deliberative vs. Automatic Nursing Actions: Understanding when to use deliberate, problem-solving actions versus routine, automatic responses is crucial to effective nursing practice.
- Prioritization of Immediate Needs: Orlando’s theory emphasizes distinguishing urgent needs that require immediate intervention from those that can be planned for long-term care.
- Effective Communication Enhances Care Outcomes: Accurately interpreting verbal and non-verbal patient cues leads to targeted, successful interventions and better patient outcomes.
- Adaptability and Evaluation: Continuous assessment and evaluation of interventions ensure that patient care remains effective and responsive to changing needs.
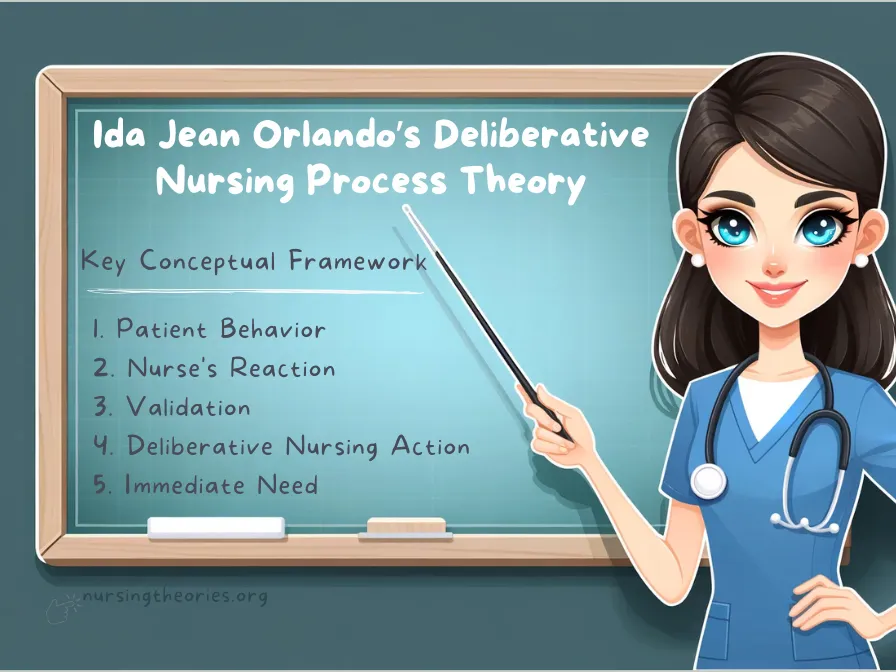
Core Concepts of Ida Jean Orlando’s Deliberative Nursing Process Theory
Ida Jean Orlando’s Deliberative Nursing Process Theory focuses on dynamic nurse-patient interactions, where nursing actions are deliberate and based on validated patient needs.
The theory ensures that nurses understand, prioritize, and address patient distress effectively through personalized care.
Here’s a closer look at its core components:
1) Patient Behavior: The Communication of Needs
Patient behavior includes both verbal and non-verbal cues that signal underlying health concerns or distress.
Every patient behavior is a meaningful form of communication that requires careful observation and interpretation.
These signals can be:
- Explicit: Verbal complaints or direct statements such as “I feel pain.”
- Implicit: Non-verbal cues like grimacing, restlessness, or changes in posture.
Example: A patient clutching their abdomen and wincing without saying a word communicates possible pain or discomfort, prompting further assessment.
Key Insight: Recognizing patient behavior as a starting point for care ensures that no need goes unnoticed, enabling early intervention.
Think of it as… A text message from the body—silent or spoken, it conveys valuable information that requires decoding.
2) Nurse’s Reaction: Perceptive Interpretation
The nurse’s initial perception and internal interpretation of patient behavior.
The nurse forms an initial understanding of the patient’s needs based on observation, but this interpretation must always be validated to prevent errors.
Process:
- Observe: Identify patient behaviors or cues.
- Form an Initial Hypothesis: Develop an idea of what the behavior may indicate.
- Validate: Seek confirmation by directly communicating with the patient to avoid incorrect assumptions.
Example: If a nurse observes a patient grimacing, they may initially think it’s related to post-operative pain.
However, they should confirm this by asking, “Are you experiencing pain, or is it something else?”
Key Insight: The nurse’s reaction ensures they remain perceptive to the patient’s needs while using validation to enhance accuracy.
Think of it as… Reading a map—you see the path ahead but verify the directions before continuing.
3) Validation: Confirming Understanding
The process of directly verifying that the nurse’s interpretation of the patient’s needs is correct.
Assumptions can lead to errors, so validation through active communication is critical for accurate care.
Approach:
- Ask Open-Ended Questions: “Can you describe what you’re feeling?”
- Listen Actively: Pay close attention to patient responses.
- Verify Initial Observations: Confirm the accuracy of the nurse’s perception.
- Adjust as Needed: Modify care plans based on patient feedback.
Example: A nurse might observe a patient shifting uncomfortably in bed and say, “You seem uncomfortable—can you tell me what’s bothering you?” The patient may then clarify whether it’s pain, stiffness, or another issue.
Key Insight: Validation ensures that nursing interventions target the correct problem, minimizing unnecessary or ineffective treatments.
Think of it as… Double-checking a recipe before baking to avoid adding the wrong ingredient.
4) Deliberative Nursing Action: Personalized Intervention
Purposeful, patient-specific actions developed through careful assessment and validation of patient needs.
Interventions should be individualized and responsive rather than routine or automatic.
Deliberative actions ensure that care addresses the patient’s immediate concerns effectively.
Characteristics:
- Targeted and Specific: Tailored to the unique needs of the patient.
- Flexible and Responsive: Adjusted based on ongoing assessments.
- Validated: Rooted in confirmed patient communication.
Example: After confirming that a patient is experiencing abdominal pain, the nurse may take specific actions such as administering pain medication, adjusting the patient’s position, or notifying the healthcare provider.
Key Insight: Deliberative actions are more effective because they are intentional and focused on the patient’s validated needs, avoiding unnecessary interventions.
Think of it as… Customizing a workout plan based on individual fitness goals rather than following a generic routine.
5) Immediate Need: Prioritizing Patient Distress
The most urgent issue requiring prompt nursing intervention to relieve patient distress.
Addressing immediate needs is crucial for preventing complications and ensuring patient stabilization.
Once the immediate concern is resolved, nurses can develop long-term care plans.
Strategy:
- Identify the Critical Issue: Determine the most pressing concern through observation and validation.
- Provide Immediate Relief: Deliver rapid interventions such as pain management or oxygen therapy.
- Stabilize Before Expanding Care: Once the immediate need is addressed, additional assessments and planning can take place.
Example: A patient experiencing severe shortness of breath should receive oxygen therapy immediately to alleviate distress before investigating the cause.
Key Insight: Prioritizing immediate needs ensures that critical conditions are managed promptly, promoting patient safety and recovery.
Think of it as… Putting out a fire before investigating its cause—urgent action comes first to prevent harm.
Critical Distinctions in Orlando’s Nursing Process
I) Immediate vs Delayed Needs in Patient Care
Orlando emphasizes the importance of prioritizing immediate needs over delayed ones.
- Immediate Needs: These require urgent intervention to alleviate acute distress and prevent complications.
- Example: Administering pain relief to a patient in severe pain or oxygen to a patient struggling to breathe.
- Delayed Needs: These involve long-term care and follow-up interventions once the patient is stable.
- Example: Educating a patient on managing diabetes after their immediate symptoms have been controlled.
Key Insight: Differentiating between urgent and long-term needs ensures that patient care is efficient and effective.
Think of it as… Treating a wound before worrying about the scar—address the critical issue first.
II) Deliberative vs Automatic Nursing Actions
Orlando distinguishes between two types of nursing actions:
- Deliberative Actions: Thoughtful and patient-specific, based on validated assessments.
- Example: Administering pain medication only after confirming the patient’s discomfort level.
- Automatic Actions: Routine responses based on protocols, often performed without validating the patient’s immediate need.
- Example: Automatically checking vital signs as part of a shift change without asking the patient how they feel.
Key Insight: Deliberative actions enhance patient outcomes by ensuring that interventions are targeted and meaningful.
Think of it as… Choosing between autopilot and manual control—sometimes, manual attention is needed to navigate complex situations effectively.
The Evolution of the Traditional Nursing Process
While Orlando laid the groundwork for dynamic, patient-centered care, nursing practice has since developed a more structured, systematic approach to patient care.
The traditional nursing process emerged as a comprehensive framework that builds upon Orlando’s foundational principles.
Five-Step Nursing Process
- Assessment
- Comprehensive data collection about the patient’s health status
- Involves multiple methods:
- Patient interviews
- Physical examinations
- Review of medical history
- Diagnostic test results
- Aims to gather holistic information about the patient’s current condition
- Diagnosis
- Identifying specific health problems or potential risks
- Analyzing assessment data to:
- Recognize actual health issues
- Identify potential complications
- Determine patient’s specific nursing care needs
- Creates a clear foundation for targeted interventions
- Planning
- Developing a strategic, individualized care plan
- Key activities include:
- Setting precise, measurable patient care goals
- Prioritizing interventions
- Collaborating with the patient and healthcare team
- Designing specific nursing interventions
- Implementation
- Executing the planned nursing interventions
- Involves:
- Carrying out nursing actions
- Coordinating care with other healthcare professionals
- Documenting patient responses
- Adapting interventions as needed
- Evaluation
- Analyzing the effectiveness of nursing interventions
- Processes include:
- Comparing patient outcomes to initial goals
- Assessing the impact of nursing actions
- Modifying the care plan based on patient progress
- Continuous quality improvement
Connecting Orlando’s Theory to the Traditional 5-Step Nursing Process
Orlando’s original theory remains the philosophical backbone of this structured approach.
The traditional nursing process incorporates her key insights:
- Patient-Centered Care: Maintains focus on individual patient needs
- Dynamic Communication: Emphasizes continuous patient interaction
- Personalized Interventions: Encourages tailored, responsive care
- Immediate Need Recognition: Prioritizes addressing urgent patient concerns
Applying Orlando’s Deliberative Nursing Process Theory to Problem-Based Care
Step 1: Assessing Patient Behavior for Effective Nursing Intervention
The first step in applying Orlando’s theory involves recognizing and interpreting patient behaviors, which often reveal unmet needs.
Nurses gather information through observation, listening, and questioning to uncover the underlying cause of the patient’s behavior.
Example: A post-op patient may not explicitly state they are in pain but may show signs like moaning, sweating, or avoiding movement.
Recognizing these cues prompts further assessment to provide relief.
Key Insight: Effective assessment involves paying attention to both verbal and non-verbal cues to fully understand the patient’s condition.
Think of it as… Detecting early warning signals that guide the next steps in care.
Step 2: Interpreting Nurse Reactions to Patient Cues
Once patient cues are identified, the nurse must interpret their meaning and determine the appropriate reaction.
This step involves differentiating between immediate needs and those that can be addressed later.
Example: A patient complaining of dizziness may be showing signs of low blood sugar, dehydration, or medication side effects.
The nurse reacts by checking vital signs and blood glucose levels to identify the correct intervention.
Key Insight: Accurate interpretation ensures that nurses respond with interventions that directly address the patient’s problem.
Think of it as… Analyzing the clues in a mystery—each response leads to uncovering the root cause.
Step 3: Implementing Deliberative Nursing Actions to Meet Patient Needs
Deliberative nursing actions, guided by assessment and interpretation, are designed to meet the specific needs of the patient.
These actions require critical thinking and collaboration with other healthcare professionals when necessary.
Example: After identifying dehydration as the cause of a patient’s dizziness, the nurse administers fluids and monitors electrolyte levels while coordinating with the physician.
Key Insight: Deliberative actions ensure that care is tailored to the patient’s unique condition and needs, enhancing the likelihood of positive outcomes.
Think of it as… Executing a well-planned strategy that adapts as new information emerges.
The Nursing Process Framework in Ida Jean Orlando’s Theory
Step 1: Assessing Patient Cues and Behavior
The nurse begins by collecting comprehensive data from the patient’s verbal and non-verbal cues, behaviors, and responses.
This step is crucial for understanding the patient’s current needs and potential issues.
Example: A patient with chronic pain may exhibit signs of discomfort, such as shifting in bed or wincing, even without verbalizing pain.
The nurse observes these behaviors and collects additional information through questioning and medical history review.
Key Insight: Gathering data helps the nurse gain a holistic understanding of the patient’s situation and establish a strong foundation for diagnosis and intervention.
Think of it as… Building a puzzle—each observation is a piece that contributes to the complete picture of the patient’s condition.
Step 2: Formulating a Nursing Diagnosis Based on Behavioral Cues
After gathering and interpreting patient data, the nurse develops a nursing diagnosis by identifying problems or unmet needs.
The diagnosis guides the development of a care plan and interventions.
Example: A patient showing signs of restlessness and high blood pressure may be diagnosed with anxiety due to impending surgery.
Key Insight: A clear and accurate nursing diagnosis ensures that the care plan addresses the most pressing issues affecting the patient.
Think of it as… Diagnosing the underlying cause before prescribing a solution, similar to troubleshooting a technical issue.
Step 3: Developing a Patient-Centered Care Plan
Once the diagnosis is established, the nurse collaborates with the patient to create a care plan.
This step involves setting realistic goals and selecting appropriate interventions tailored to the patient’s needs.
Example: For a patient with anxiety about surgery, the care plan may include relaxation exercises, therapeutic communication, and pre-operative counseling.
Key Insight: Collaboration ensures that the care plan is personalized, achievable, and aligned with the patient’s preferences.
Think of it as… Drawing a personalized map—each route is designed to reach the final goal of improved health outcomes.
Step 4: Implementing Nursing Interventions for Targeted Care
The nurse carries out the interventions identified in the care plan while remaining flexible to adjust actions based on the patient’s response.
This step often involves coordinating with other healthcare team members.
Example: For a patient experiencing pain, the nurse may administer pain medication, provide comfort measures, and offer emotional support.
Key Insight: Effective implementation requires flexibility and adaptability, as patients’ needs may evolve during care.
Think of it as… Following a recipe but being ready to adjust ingredients to achieve the best outcome.
Step 5: Evaluating the Effectiveness of Nursing Interventions
The final step involves evaluating whether the nursing interventions have successfully met the established goals.
If the desired outcomes are not achieved, the care plan is reassessed, and modifications are made.
Example: If a patient’s anxiety persists despite counseling, the nurse may involve a psychologist or adjust the interventions to include relaxation techniques.
Key Insight: Continuous evaluation ensures that the nursing care remains relevant and effective as the patient’s condition changes.
Think of it as… Monitoring progress on a road trip and recalculating the route if necessary to reach the destination.
Case Studies Using Orlando’s Nursing Process Theory
Case Study 1: Managing Post-Surgical Pain with Nurse-Patient Interaction
Scenario: A 60-year-old patient is recovering from abdominal surgery.
Although they deny severe pain verbally, the nurse notices signs of discomfort, including grimacing, restlessness, and shallow breathing.
Application of Orlando’s Theory:
- Assessment: The nurse observes the patient’s non-verbal cues and asks questions to understand the intensity of the pain.
- Diagnosis: Based on behavioral cues, the nurse diagnoses post-operative pain as the primary issue.
- Intervention: The nurse administers prescribed pain relief and positions the patient comfortably while providing emotional support.
- Evaluation: The patient’s vital signs stabilize, and their body language indicates relaxation. Follow-up assessments are conducted to ensure sustained comfort.
Key Insight: Recognizing pain through non-verbal cues and acting accordingly highlights the importance of ongoing nurse-patient interaction.
Think of it as… Listening to what isn’t said—non-verbal communication often reveals crucial information about patient needs.
Case Study 2: Reducing Pediatric Anxiety Through Deliberative Nursing Actions
Scenario: A 7-year-old child is admitted to the hospital for appendectomy.
The child appears visibly frightened, clings to their parent, and refuses to speak to the healthcare team.
Application of Orlando’s Theory:
- Assessment: The nurse observes the child’s behaviors, such as crying and avoidance, and talks to the parent to gather additional information.
- Diagnosis: The nurse diagnoses pre-operative anxiety as a result of fear of surgery and separation from their parent.
- Intervention: The nurse uses therapeutic communication, engages the child with age-appropriate games, and arranges for the parent to stay with the child during certain procedures.
- Evaluation: The child becomes more cooperative and less anxious, as observed through improved interaction and calm behavior.
Key Insight: Deliberative actions, such as understanding and addressing the root cause of anxiety, promote positive outcomes in pediatric care.
Think of it as… Entering the child’s world—meeting them where they are emotionally and providing comfort in a relatable way.
Case Study 3: Enhancing Communication with Non-Verbal Patients Using Orlando’s Theory
Scenario: A stroke patient with aphasia is unable to communicate verbally, creating a barrier to expressing needs effectively.
Application of Orlando’s Theory:
- Assessment: The nurse observes body language, facial expressions, and gestures while also using communication boards and assistive devices.
- Diagnosis: The nurse identifies ineffective communication and emotional frustration as key issues.
- Intervention: The nurse teaches the patient how to use non-verbal communication tools, ensuring the patient can express discomfort or requests.
- Evaluation: The patient successfully communicates pain levels and other needs, leading to improved collaboration in care.
Key Insight: Nurses can adapt their communication strategies to bridge gaps and ensure patients have a voice in their care.
Think of it as… Speaking the patient’s language—finding alternative ways to understand their needs when words aren’t available.
Modern Relevance of Orlando’s Nursing Process Theory
Enhancing Patient Safety Through Accurate Assessment of Behavioral Cues
Orlando’s theory plays a critical role in enhancing patient safety by ensuring that nurses identify and address problems as they arise.
By focusing on both verbal and non-verbal cues, nurses can detect early signs of complications or distress that might otherwise go unnoticed.
Example: A patient showing signs of respiratory distress through labored breathing and confusion may receive immediate oxygen therapy before their condition worsens.
Key Insight: Early detection and intervention prevent complications and improve patient outcomes.
Think of it as… Catching a spark before it becomes a fire—quick response minimizes risks.
Promoting Patient-Centered Care Through Nurse-Patient Interaction
Orlando’s emphasis on dynamic interaction aligns perfectly with modern trends in patient-centered care.
By continuously engaging with patients, nurses ensure that care plans are tailored to their unique needs and preferences.
Example: For a patient with diabetes, discussing lifestyle changes and collaboratively setting achievable goals improves adherence to treatment.
Key Insight: Individualized care fosters trust and collaboration, leading to better compliance and health outcomes.
Think of it as… Co-piloting a journey—patients are active participants in their healthcare.
Integrating Evidence-Based Practice with Orlando’s Nursing Process Model
Orlando’s theory complements evidence-based nursing by linking patient assessments to informed decision-making and interventions.
Through continuous interaction, nurses can apply evidence-based solutions while adapting them to real-time patient needs.
Example: A patient experiencing post-surgical pain receives a combination of pharmacological and non-pharmacological interventions, such as relaxation techniques or guided imagery, based on evidence of their effectiveness.
Key Insight: Evidence-based practice ensures that interventions are grounded in research and tailored to individual patients.
Think of it as… Combining science and empathy—using research-backed interventions while addressing the human side of care.
Challenges and Limitations of Applying Orlando’s Deliberative Nursing Process Theory
Time Constraints in Fast-Paced Clinical Environments
In high-pressure healthcare settings, nurses may find it challenging to allocate sufficient time to assess patient behaviors thoroughly and respond with deliberative actions.
The need for quick decisions often leads to automatic responses, which may overlook patient-specific needs.
Example: In an emergency room, nurses may have limited time to engage with a patient displaying non-verbal distress, potentially delaying the identification of an underlying issue.
Key Insight: Time constraints can hinder the application of individualized, patient-centered care.
Think of it as… Trying to read a novel in a rush—you may miss critical details when time is limited.
Risk of Misinterpreting Patient Behavior in Complex Cases
Patients with complex medical or psychological conditions may present ambiguous behaviors that can be misinterpreted, leading to incorrect assessments and interventions.
This is especially true in cases involving non-verbal or cognitively impaired patients.
Example: A patient with dementia exhibiting agitation may be misdiagnosed as experiencing pain, when in fact, the behavior could be due to environmental triggers or unmet social needs.
Key Insight: Misinterpretation of patient cues can result in ineffective or inappropriate care interventions.
Think of it as… Misreading signals on a GPS—incorrect interpretation can take you off course.
Balancing Deliberative and Automatic Nursing Actions in Patient Care
While Orlando’s theory emphasizes the importance of deliberative actions, not all situations allow for them.
Nurses must find a balance between routine, efficient responses and the intentional problem-solving approach Orlando advocates.
Example: During a routine assessment, a nurse might rely on automatic checks for vital signs but switch to deliberative action when a patient expresses unexpected symptoms.
Key Insight: Balancing the two types of nursing actions requires clinical judgment and flexibility to adapt based on patient needs and the situation.
Think of it as… Switching between manual and automatic gears—knowing when to engage deeper critical thinking is crucial for effective care.
Ida Jean Orlando’s Deliberative Nursing Process Theory Quiz
1) What is the primary focus of Ida Jean Orlando’s Nursing Process Theory?
a) Developing standardized care plans
b) Reducing the role of patient communication
c) Addressing patient needs through continuous nurse-patient interaction
d) Prioritizing routine, automatic actions over personalized care
2) Which of the following best describes a deliberative nursing action in Orlando’s model?
a) Automatically checking vital signs
b) Responding to a patient’s pain complaint by adjusting medication
c) Completing documentation without patient interaction
d) Performing hygiene care as part of a daily routine
3) How does Orlando’s theory differentiate immediate needs from delayed needs?
a) Immediate needs require long-term planning and delayed intervention
b) Immediate needs are identified through assessment and require urgent action
c) Delayed needs always take priority over immediate concerns
d) Delayed needs do not involve patient participation
4) What is a key challenge when applying Orlando’s theory in fast-paced clinical settings?
a) Lack of access to medical equipment
b) Limited opportunities to establish nurse-patient interaction
c) Excessive documentation requirements
d) Difficulty in prioritizing non-verbal cues
5) Why is accurate interpretation of patient behavior crucial in Orlando’s Nursing Process Theory?
a) It reduces the need for follow-up care
b) It ensures routine tasks are completed on time
c) It guides tailored interventions to address patient-specific issues
d) It eliminates the need for collaborative care
Ida Jean Orlando’s Nursing Process Theory Quiz Answers with Rationale
- Correct Answer: c) Addressing patient needs through continuous nurse-patient interaction
Rationale: Orlando’s theory centers on dynamic interaction between the nurse and patient to assess, identify, and meet individualized needs. - Correct Answer: b) Responding to a patient’s pain complaint by adjusting medication
Rationale: Deliberative actions require intentional responses tailored to the patient’s specific needs, unlike routine or automatic actions. - Correct Answer: b) Immediate needs are identified through assessment and require urgent action
Rationale: Immediate needs are critical and must be addressed promptly, whereas delayed needs can be planned for future interventions. - Correct Answer: b) Limited opportunities to establish nurse-patient interaction
Rationale: In fast-paced settings, time constraints often limit the ability to assess patient behavior thoroughly and respond with individualized care. - Correct Answer: c) It guides tailored interventions to address patient-specific issues
Rationale: Accurate interpretation of patient behavior ensures that interventions are appropriate and directly address the underlying problem.
Questions and Answers on Orlando’s Nursing Process Theory
Q1: What role does patient behavior play in Orlando’s Nursing Process Theory?
A: Patient behavior serves as a cue for nurses to assess and identify immediate or delayed needs, guiding the development of personalized care.
Q2: How do nurses balance deliberative and automatic actions in care delivery?
A: Nurses rely on routine actions for efficiency but prioritize deliberate, thoughtful responses when patient cues indicate specific needs.
Q3: How can Orlando’s theory enhance patient-centered care?
A: By promoting continuous interaction and assessment, nurses can provide care that is tailored to the individual’s real-time needs and preferences.
Q4: What is an example of misinterpreting patient behavior in practice?
A: Assuming a patient’s agitation is due to pain when it is actually caused by anxiety or an environmental factor could result in ineffective interventions.
Q5: Why is ongoing evaluation important in Orlando’s framework?
A: Continuous evaluation ensures that nursing interventions remain effective and adapt to any changes in the patient’s condition.
Conclusion of Ida Jean Orlando’s Nursing Process Theory
Ida Jean Orlando’s Deliberative Nursing Process Theory underscores the importance of real-time, dynamic nurse-patient interaction in delivering effective, patient-centered care.
For nurses aiming to enhance their problem-solving skills, Orlando’s framework offers a flexible approach that prioritizes individual patient outcomes.
Its application in diverse settings—from emergency rooms to long-term care units—demonstrates its versatility and lasting impact on modern nursing practice. Learn more about Ida Jean Orlando here.
Final Reflective Question: How can nurses effectively balance the demands of fast-paced clinical environments with the need for deliberative, patient-centered care as outlined in Orlando’s Nursing Process Theory?