Hildegard Peplau, often referred to as the “mother of psychiatric nursing,” revolutionized mental health care with her development of the Interpersonal Relations Theory.
Her work shifted the focus of nursing beyond clinical tasks and emphasized the significance of therapeutic communication and the nurse-patient relationship.
Peplau believed that by forming meaningful connections, nurses could guide patients through their healing journeys and help them gain insight into their emotions and behaviors.
Read Hildegard Peplau’s biography here.
This article will explore how Peplau’s theory can be applied to psychiatric nursing, particularly in managing mental health disorders through therapeutic communication and real-world case examples.
What You’ve Learned – Hildegard Peplau’s Interpersonal Relations Theory
- The nurse-patient relationship is a powerful therapeutic tool: Peplau’s theory focuses on how communication and collaboration between nurses and patients facilitate healing.
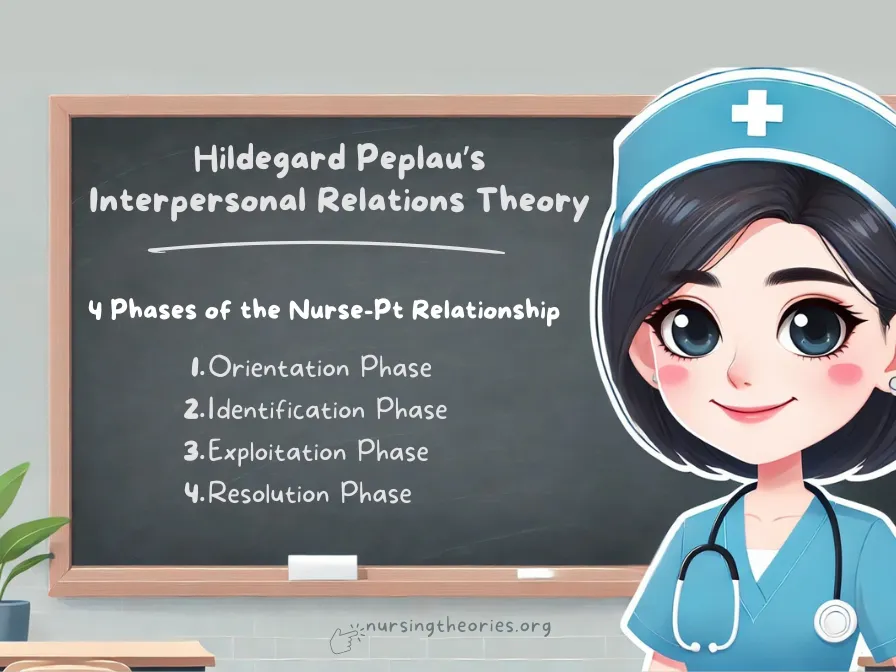
- The four phases of the nurse-patient relationship guide care delivery: These phases—orientation, identification, exploitation, and resolution—ensure that care progresses systematically.
- Nurses adopt multiple roles to meet patients’ needs: Peplau outlined six key roles, including teacher, counselor, and leader, that nurses use to provide holistic care.
- Therapeutic communication is central to mental health recovery: Techniques like active listening, empathy, and nonverbal communication foster trust and emotional expression.
- Peplau’s theory extends beyond psychiatry: Although developed for psychiatric nursing, its principles are applicable in various settings, including chronic care, community health, and primary care.
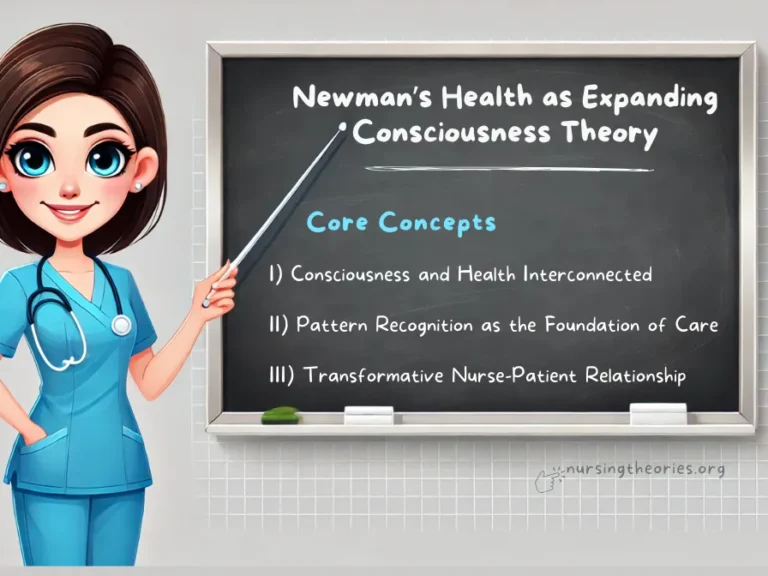
Core Concepts of Peplau’s Interpersonal Relations Theory
The Nurse-Patient Relationship as the Core of Peplau’s Theory
At the heart of Peplau’s theory is the belief that the nurse-patient relationship serves as a therapeutic tool to promote mental health recovery.
Unlike traditional models that viewed patients as passive recipients of care, Peplau’s theory emphasized active collaboration between the nurse and the patient.
The relationship is built on mutual respect, empathy, and trust, where both parties work together to identify the patient’s needs and develop coping mechanisms.
The success of this relationship depends on the nurse’s ability to create a safe and supportive environment that encourages open communication.
Key Insight: By fostering therapeutic connections, nurses help patients explore their emotions, overcome challenges, and regain their independence.
Think of it as… A partnership where both the nurse and patient contribute to achieving healing and recovery.
The Four Phases of the Nurse-Patient Relationship
Peplau outlined four distinct phases that guide the progression of the nurse-patient relationship:
- Orientation Phase: The nurse introduces themselves and establishes trust by gathering information about the patient’s needs. The goal is to create a sense of security and lay the foundation for collaboration.
- Identification Phase: The patient begins to recognize their problems, and the nurse supports them by offering guidance and resources. This phase is marked by active engagement in problem-solving.
- Exploitation Phase: The patient takes advantage of available services and resources to work toward their goals. The nurse continues to provide support and monitor progress.
- Resolution Phase: The relationship comes to an end as the patient’s problems are resolved or managed. The patient regains independence and is ready to transition to self-care.
Key Insight: Each phase plays a vital role in ensuring that the patient’s journey toward recovery is structured, supportive, and goal-oriented.
Think of it as… A four-step bridge that helps the patient transition from dependence to independence.
The Six Nursing Roles in Peplau’s Theory
Peplau identified six key roles that nurses adopt throughout the therapeutic process:
- Stranger: The nurse initially approaches the patient with openness and a willingness to listen.
- Resource Person: The nurse provides information and answers questions to help the patient make informed decisions.
- Teacher: The nurse educates the patient about their condition and coping strategies.
- Counselor: The nurse offers emotional support and helps the patient explore their feelings.
- Surrogate: The nurse may temporarily take on a parental or guiding role, especially when the patient feels vulnerable.
- Leader: The nurse guides the patient toward their goals by promoting active participation in their care.
Key Insight: The ability to switch between roles allows nurses to address various aspects of patient care, from emotional support to practical problem-solving.
Think of it as… Wearing multiple hats to meet the changing needs of the patient.
Therapeutic Communication in Peplau’s Interpersonal Relations Theory
Importance of Active Listening and Empathy
Therapeutic communication begins with active listening—the ability to listen attentively, without judgment, and respond in a way that shows understanding.
Empathy is crucial, as it allows the nurse to connect with the patient’s emotional experience and provide meaningful support.
Example: A nurse working with a patient diagnosed with severe anxiety listens to their fears without interrupting and responds with validation, such as, “It’s okay to feel overwhelmed.
Let’s explore ways to ease your anxiety.”
Key Insight: Active listening builds trust and encourages patients to open up about their thoughts and feelings.
Think of it as… Providing a safe space where the patient feels heard and valued.
Using Open-Ended Questions to Facilitate Exploration
Open-ended questions are designed to encourage patients to express themselves fully, rather than providing one-word answers.
They help uncover deeper emotional issues and foster reflection.
Example: A psychiatric nurse might ask, “Can you tell me more about how you felt during the panic attack?” instead of asking, “Did you feel scared?”
Key Insight: Open-ended questions facilitate meaningful conversations and allow the nurse to gain a comprehensive understanding of the patient’s concerns.
Think of it as… Opening a door that invites the patient to share their experiences freely.
Nonverbal Communication as a Therapeutic Tool
Nonverbal communication, such as body language, facial expressions, and posture, plays a significant role in conveying empathy and understanding.
Maintaining eye contact, nodding, and sitting at the patient’s level can enhance verbal communication.
Example: A nurse sitting next to a distressed patient and gently placing a hand on their shoulder can convey support without the need for words.
Key Insight: Nonverbal cues complement verbal communication and reinforce the nurse’s compassionate presence.
Think of it as… Speaking a silent language of care that the patient can understand and feel.
Applying the Nursing Process in Peplau’s Interpersonal Relations Theory
Step 1: Assessment through Therapeutic Interaction
The first step of the nursing process involves gathering information about the patient’s emotional, mental, and physical state.
In Peplau’s framework, the assessment phase heavily relies on therapeutic communication to uncover underlying issues that may not be obvious through observation alone.
Example: A nurse assessing a patient with depression asks open-ended questions about their mood, sleep patterns, and recent experiences while observing nonverbal cues like body posture and facial expressions.
Key Insight: The quality of assessment improves when patients feel comfortable sharing their feelings, making therapeutic interaction essential.
Think of it as… Peeling back layers to reach the root of the problem through gentle, compassionate inquiry.
Step 2: Identifying Problems and Setting Goals
Once the nurse has gathered sufficient information, they work collaboratively with the patient to identify specific problems and set realistic, achievable goals.
Peplau emphasized that goal-setting should be done together to foster patient engagement and ownership of the healing process.
Example: A patient with social anxiety agrees with the nurse to set a goal of attending a small group therapy session by the end of the week.
Key Insight: Joint goal-setting ensures that patients are active participants in their care, increasing the likelihood of success.
Think of it as… Creating a roadmap for recovery with input from both the nurse and the patient.
Step 3: Planning Therapeutic Interventions
The nurse develops a care plan with interventions tailored to the patient’s specific needs, incorporating both clinical treatments and emotional support strategies.
Interventions may involve counseling sessions, coping mechanisms, or referral to specialized services.
Example: For a patient struggling with anger management, the nurse may schedule daily reflection sessions where the patient discusses their triggers and learns coping techniques like deep breathing.
Key Insight: Personalized care plans address not only symptoms but also emotional triggers, promoting comprehensive healing.
Think of it as… Designing a customized care blueprint that adapts to the patient’s evolving needs.
Step 4: Implementing Interventions through the Phases of the Nurse-Patient Relationship
The interventions are carried out while the nurse and patient navigate the phases of the nurse-patient relationship—from trust-building in the orientation phase to patient growth in the exploitation and resolution phases.
Example: A nurse working with a PTSD patient might begin by creating a safe, trusting environment (orientation), gradually guiding the patient to explore trauma-related memories (identification), and providing therapeutic tools like relaxation exercises (exploitation).
Key Insight: Progress through the phases ensures that interventions build on each other, fostering sustainable improvement.
Think of it as… Climbing a ladder, where each step is supported by the foundation laid in previous interactions.
Step 5: Evaluation and Reflection
The final step is evaluating whether the interventions have achieved the desired outcomes.
This involves assessing changes in the patient’s emotional state, behavior, and progress toward their goals.
If necessary, the nurse and patient can revise the care plan.
Example: If a patient with anxiety shows improvement in managing panic attacks but continues to struggle with social interactions, the nurse may adjust the plan to include social exposure therapy.
Key Insight: Regular evaluation allows for flexible, patient-centered care that evolves based on the patient’s progress.
Think of it as… Checking the compass during a journey to ensure the right path is being followed and making adjustments if needed.
Real-World Applications of Peplau’s Theory in Psychiatric Nursing
Case Study 1: Managing Anxiety Disorders
A psychiatric nurse working with a patient experiencing generalized anxiety disorder (GAD) begins by establishing trust in the orientation phase.
Through therapeutic communication, the patient identifies their primary triggers, such as social gatherings.
During the exploitation phase, the nurse introduces coping strategies, including deep breathing exercises and positive affirmations.
By the resolution phase, the patient feels confident enough to attend small social events without experiencing severe anxiety.
Case Study 2: Addressing Depression through Goal-Oriented Therapy
A patient with severe depression is initially withdrawn and reluctant to engage.
The nurse starts by building trust in the orientation phase, offering a safe space for the patient to express their feelings.
As they progress to the identification phase, the patient sets a goal of completing small daily tasks, such as taking a short walk.
By the resolution phase, the patient is more independent and shows improved mood and energy levels.
Case Study 3: Building Trust in Patients with PTSD
A nurse working with a veteran diagnosed with PTSD uses Peplau’s counselor role to help the patient process traumatic experiences.
Initially, the patient resists opening up, but through nonjudgmental listening and small trust-building exercises, the nurse guides them through exposure therapy.
By the end of treatment, the patient demonstrates significant improvement in managing flashbacks and emotional responses.
Modern Implications of Peplau’s Interpersonal Relations Theory
Relevance in Psychiatric and Mental Health Nursing
Peplau’s theory remains a cornerstone of psychiatric nursing, especially in settings where building trust and promoting open communication are critical.
It continues to guide nurses in managing conditions like depression, anxiety, and schizophrenia by fostering therapeutic relationships.
Supporting Patients with Chronic Mental Illness
For patients with chronic conditions like bipolar disorder or schizophrenia, Peplau’s theory helps establish long-term therapeutic relationships that support sustained progress.
The collaborative approach ensures that patients receive ongoing emotional support and guidance.
Enhancing Communication Skills Across Healthcare Settings
Peplau’s model is not limited to psychiatric nursing—it has been applied in community health, primary care, and even palliative care settings.
Effective communication is central to any healthcare setting, and Peplau’s emphasis on therapeutic interaction benefits patients across various disciplines.
Challenges and Limitations of Peplau’s Interpersonal Relations Theory
Time Constraints in Building Trust
In fast-paced clinical environments, nurses may find it difficult to establish meaningful relationships with patients due to time limitations.
Shorter interactions can hinder the depth of therapeutic engagement.
Patient Resistance or Communication Barriers
Some patients may be unwilling or unable to engage in therapeutic communication, particularly if they have trust issues, language barriers, or severe psychiatric conditions.
Balancing Professional Boundaries
While building trust is essential, maintaining professional boundaries can be challenging.
Nurses must strike a balance between showing empathy and avoiding over-involvement, which can lead to emotional burnout.
Peplau’s Interpersonal Relations Theory Quiz
1) What is the primary focus of Peplau’s Interpersonal Relations Theory?
a) Administering medication
b) Building therapeutic nurse-patient relationships
c) Conducting diagnostic tests
d) Developing surgical interventions
2) What is the first phase of the nurse-patient relationship in Peplau’s theory?
a) Exploitation
b) Resolution
c) Orientation
d) Identification
3) Which nursing role involves providing emotional support to patients?
a) Leader
b) Counselor
c) Teacher
d) Resource person
4) What is a key communication strategy emphasized in Peplau’s theory?
a) Using medical jargon
b) Active listening
c) Quick conversations
d) Non-engagement
4) How can Peplau’s theory benefit patients with chronic mental illness?
a) By focusing only on short-term goals
b) By establishing long-term therapeutic relationships
c) By avoiding communication
d) By limiting patient involvement
Peplau’s Interpersonal Relations Theory Quiz Answers with Rationale
- Correct Answer: b) Building therapeutic nurse-patient relationships
Rationale: Peplau’s theory centers on the nurse-patient relationship as the main therapeutic tool for healing. - Correct Answer: c) Orientation
Rationale: The orientation phase is the initial phase where trust is established and the patient’s needs are identified. - Correct Answer: b) Counselor
Rationale: The counselor role focuses on providing emotional support and helping patients explore their feelings. - Correct Answer: b) Active listening
Rationale: Active listening is a key component of therapeutic communication, allowing patients to express their thoughts without judgment. - Correct Answer: b) By establishing long-term therapeutic relationships
Rationale: Long-term therapeutic relationships provide ongoing support, which is essential for managing chronic mental health conditions.
Questions and Answers on Peplau’s Interpersonal Relations Theory
Q1: What is the purpose of the four phases in Peplau’s theory?
A: To guide the nurse-patient relationship from initial trust-building to resolution and patient independence.
Q2: How does Peplau’s theory apply in non-psychiatric settings?
A: Its principles of communication and collaboration are useful in settings like community health, palliative care, and chronic disease management.
Q3: Why are professional boundaries important in Peplau’s model?
A: They ensure that nurses maintain empathy without becoming emotionally over-involved or experiencing burnout.
Q4: What is the role of open-ended questions in therapeutic communication?
A: They encourage patients to share their experiences and feelings in detail, promoting emotional exploration.
Q5: How do the six nursing roles benefit patient care?
A: They provide flexibility, allowing nurses to address diverse patient needs through roles like counselor, teacher, and resource person.
Conclusion of Peplau’s Interpersonal Relations Theory
Hildegard Peplau’s Interpersonal Relations Theory highlights the transformative power of the nurse-patient relationship in promoting healing.
By using therapeutic communication, active listening, and collaboration, nurses can help patients navigate mental health challenges and achieve better emotional well-being.
As nursing continues to evolve, Peplau’s theory remains a vital guide for fostering compassionate, patient-centered care.
Final Reflective Question: How can nurses integrate Peplau’s therapeutic communication techniques into fast-paced clinical settings while maintaining efficiency?