Florence Nightingale’s Environmental Theory is much more than a historical relic—it remains relevant in modern nursing practice, influencing infection control protocols, hospital design, and patient care standards.
In this article, we’ll break down the core principles of the theory, explore the key environmental factors Nightingale emphasized, and demonstrate how they continue to guide nursing practice today.
What You’ve Learned
- The environment is central to healing and recovery: Nightingale’s Environmental Theory emphasizes clean air, water, sanitation, and adequate lighting as critical factors for preventing disease and promoting recovery.
- Nurses play a vital role as environmental managers: From maintaining hygiene to controlling noise levels, nurses are responsible for creating optimal conditions that support patient well-being.
- Cleanliness and sanitation remain pillars of modern healthcare: Nightingale’s focus on proper waste disposal, disinfection, and hand hygiene continues to shape today’s infection control protocols.
- Environmental management extends beyond physical care: Nightingale’s holistic vision includes psychological and emotional well-being, making natural light, quiet spaces, and comfort essential to recovery.
- Her theory is still relevant to modern challenges: Whether addressing hospital-acquired infections, pandemic responses, or sustainable healthcare practices, Nightingale’s principles remain a timeless guide for improving patient outcomes.
Core Principles of Nightingale’s Environmental Theory
Florence Nightingale believed that the environment plays a pivotal role in a patient’s recovery.
Her Environmental Theory focuses on creating optimal conditions for healing by modifying environmental factors.
She saw the nurse as a key figure in managing these conditions, ensuring that every aspect of the environment supported the patient’s well-being.
Let’s explore the core principles that form the foundation of this influential theory.
1) The Healing Power of the Environment
Nightingale’s central idea was that health and recovery are directly influenced by the patient’s surroundings.
She observed that poor sanitation, stale air, and unclean living spaces were often responsible for worsening illness, and she believed that many diseases could be prevented by improving these environmental conditions.
Key Insight:
Nightingale viewed the environment as an integral part of patient care, making it a nurse’s responsibility to create surroundings that promote healing.
Think of it as…
The environment is like the soil for a plant’s growth—just as plants need the right conditions to thrive, so do patients need clean and supportive surroundings to recover.
2) The Role of Nurses in Environmental Management
Nightingale positioned nurses as environmental managers, responsible for ensuring that conditions like ventilation, hygiene, and noise levels were optimal for recovery.
Nurses were not just caregivers—they were “environmental engineers” who maintained a healing space that minimized stress and maximized comfort.
Practical Example:
During her time in the Crimean War, Nightingale improved hygiene, ventilation, and nutrition in overcrowded and unsanitary military hospitals.
These changes led to a significant reduction in mortality rates.
Modern Implication:
Today, nurses follow this principle by ensuring clean hospital rooms, proper hand hygiene, and infection control measures such as disinfecting high-touch surfaces.
3) Holistic Approach to Care
Nightingale’s approach to nursing was holistic, addressing both physical and psychological well-being.
She believed that a supportive environment should not only meet the patient’s physical needs but also contribute to emotional and mental comfort.
Example:
Natural light, a calm and quiet setting, and cleanliness were essential to creating a healing atmosphere, but Nightingale also recognized the importance of compassion, empathy, and reassurance in patient recovery.
Modern Reflection:
Many hospitals now incorporate healing spaces, such as gardens or quiet zones, where patients can rest and recover in soothing environments, a direct extension of Nightingale’s holistic vision.
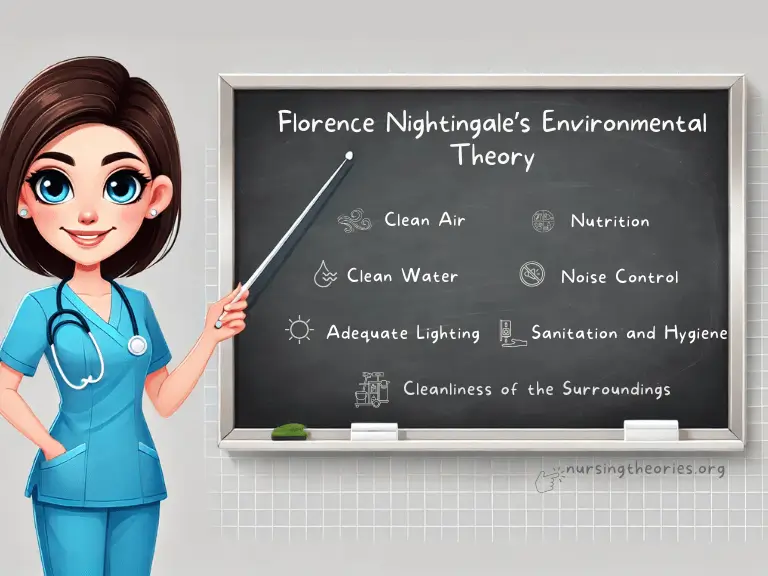
Key Environmental Factors Identified by Nightingale
Florence Nightingale identified several environmental factors that she believed directly influenced a patient’s recovery and overall well-being.
Her emphasis on cleanliness, fresh air, proper sanitation, and other key conditions became the foundation of modern healthcare standards.
Let’s explore these factors and how they continue to shape nursing practice today.
1) Clean Air
Explanation: Nightingale emphasized the importance of proper ventilation to remove stagnant air and provide fresh oxygen.
She believed that poor air circulation contributed to the spread of diseases and hindered recovery.
Modern Example:
Hospitals today use air filtration systems, HEPA filters, and proper ventilation to prevent the spread of airborne infections, such as COVID-19 or tuberculosis, especially in ICU and isolation rooms.
Key Insight:
Clean air ensures that patients breathe in oxygen-rich, pathogen-free air, supporting respiratory health and reducing infection risks.
2) Clean Water
Explanation: Nightingale stressed the need for access to safe, clean water for both drinking and hygiene.
Contaminated water was a significant cause of illness during her time, and she made its cleanliness a priority.
Modern Example:
Strict protocols are followed to ensure that water in healthcare facilities meets safety standards.
Additionally, hand hygiene programs ensure that nurses and other healthcare providers use clean water and soap to reduce the risk of infections.
Key Insight:
Clean water is essential not only for drinking but also for washing, food preparation, and infection control.
3) Sanitation and Hygiene
Explanation: Nightingale insisted on proper waste disposal, clean bedding, and general hygiene in hospital settings to prevent the spread of disease.
Modern Example:
Today’s infection control protocols, including sterilization of medical instruments and routine cleaning of hospital rooms, are rooted in Nightingale’s focus on sanitation.
Hand hygiene, the use of personal protective equipment (PPE), and disinfection of surfaces also reflect her legacy.
Think of it as…
A clean environment is like a shield, protecting patients from avoidable infections and complications.
4) Adequate Lighting
Explanation: Nightingale believed that natural light had healing properties and that a well-lit environment promoted physical and psychological well-being.
Modern Example:
Hospitals and care facilities are designed to maximize natural light exposure, reducing patient anxiety and promoting better sleep cycles.
Artificial lighting is also carefully controlled to avoid overstimulation.
Key Insight:
Light is not just about visibility—it affects mood, circadian rhythms, and overall recovery.
5) Noise Control
Explanation: Nightingale identified noise as a factor that could disturb patients, interfere with sleep, and delay recovery.
She advocated for quiet, calm environments in healthcare settings.
Modern Example:
Many hospitals have implemented “quiet hours” and soundproofing techniques to minimize unnecessary noise.
Alarms and paging systems are also regulated to reduce noise pollution.
Key Insight:
Rest is critical for healing, and minimizing noise helps patients recover faster by reducing stress and promoting restful sleep.
6) Nutrition
Explanation: Proper nutrition was one of Nightingale’s key focuses, as she believed a well-balanced diet was necessary for the body’s healing process.
Modern Example:
Today, nutritionists work with nurses and physicians to develop individualized meal plans for patients based on their medical conditions, ensuring proper nutrient intake to support recovery.
Key Insight:
Food is fuel for healing, and tailored nutrition helps optimize patient outcomes.
7) Cleanliness of the Surroundings
Explanation: Nightingale believed that the cleanliness of the patient’s surroundings—including bedding, linens, and the general environment—was essential to preventing infection and promoting healing.
Modern Example:
Hospitals follow strict cleaning protocols, ensuring that patient rooms, operating theaters, and communal areas are regularly sanitized.
Isolation rooms have enhanced cleaning protocols to protect vulnerable patients.
Think of it as…
A clean environment provides a foundation for safe, effective care, reducing the risk of hospital-acquired infections.
Real-World Examples of Nightingale’s Environmental Theory in Action
Nightingale’s Environmental Theory is more than a historical concept—it is actively applied in modern healthcare settings, with measurable improvements in patient outcomes.
Let’s look at three real-world examples that demonstrate how her principles continue to save lives and improve recovery.
Case Study 1: Infection Control in ICU Settings
Scenario: Intensive Care Units (ICUs) are highly controlled environments where patients are often vulnerable to infections due to weakened immune systems and exposure to invasive procedures.
Application of Nightingale’s Principles:
- Clean Air: Advanced air filtration systems and proper ventilation ensure a steady flow of fresh air, reducing the risk of airborne infections.
- Sanitation: Strict cleaning protocols, hand hygiene, and sterile equipment minimize the spread of pathogens.
- Noise Control: Noise-reduction measures help patients rest, which is essential for recovery.
Outcome:
A hospital that implemented enhanced infection control measures, including frequent room sanitization and noise reduction, saw a 30% decrease in hospital-acquired infections (HAIs) and faster recovery times for ICU patients.
Case Study 2: Healing Gardens in Rehabilitation Centers
Scenario: Many modern rehabilitation centers have adopted “healing gardens” as part of their environmental design to help patients recover from surgery, injury, or trauma.
Application of Nightingale’s Principles:
- Adequate Lighting: Natural sunlight is maximized to promote mood enhancement and improve the body’s natural rhythms.
- Clean Air and Ventilation: Outdoor air reduces stress and enhances respiratory function.
- Noise Control: The natural environment provides a peaceful, calming space free from disruptive hospital noises.
Outcome:
Studies have shown that patients who spend time in healing gardens experience reduced anxiety, lower blood pressure, and faster rehabilitation compared to those in traditional settings.
Key Insight:
Nightingale’s emphasis on the holistic environment extends beyond physical cleanliness to emotional and mental well-being.
Case Study 3: Disaster Relief Efforts in Underdeveloped Areas
Scenario: In the aftermath of natural disasters, displaced populations often face risks from contaminated water, lack of sanitation, and limited access to medical care.
Application of Nightingale’s Principles:
- Clean Water: Emergency teams ensure access to clean drinking water through portable purification systems.
- Sanitation: Temporary toilets and proper waste disposal facilities help reduce the spread of diseases like cholera.
- Nutrition: Relief organizations provide balanced meals to improve recovery among malnourished individuals.
Outcome:
During a flood relief mission, public health nurses helped reduce waterborne illnesses by 40% by improving access to clean water and sanitation systems.
Key Insight:
Nightingale’s principles are invaluable during crises, where environmental conditions directly affect the health of vulnerable populations.
Modern Implications of Nightingale’s Environmental Theory
While Nightingale’s Environmental Theory originated in the 19th century, its principles continue to influence modern healthcare settings.
From hospital design to pandemic responses, Nightingale’s insights remain central to creating safe, effective environments for patient care.
1) Relevance in Current Healthcare Settings
Nightingale’s emphasis on hygiene and sanitation is now embedded in standard healthcare protocols.
Infection prevention strategies, such as hand hygiene programs, routine surface disinfection, and sterile procedures, are direct applications of her ideas.
Example:
The World Health Organization’s (WHO) hand hygiene initiative, aimed at reducing healthcare-associated infections globally, reflects Nightingale’s sanitation principles.
Modern Takeaway:
Every time nurses follow handwashing protocols or disinfect patient areas, they are applying Nightingale’s environmental principles.
2) Application to Emerging Challenges
Nightingale’s theory is also relevant when addressing modern challenges, such as antimicrobial resistance and pandemic responses.
Proper environmental management—clean water, sanitation, and ventilation—reduces the spread of multidrug-resistant organisms and viral infections.
COVID-19 Response:
During the COVID-19 pandemic, hospitals applied Nightingale’s principles by improving air filtration systems, establishing isolation zones, and enforcing strict sanitation measures.
Key Insight:
Environmental management is not just a preventive measure; it’s a life-saving strategy during global health crises.
3) Sustainability and Environmental Health
Nightingale’s holistic approach to patient health can also be extended to include sustainability in healthcare.
Today’s focus on reducing hospital waste, implementing clean energy solutions, and creating eco-friendly healthcare spaces aligns with her vision of creating safe, healing environments.
Example:
Some hospitals have adopted sustainable cleaning products and waste reduction programs to minimize environmental impact without compromising hygiene and sanitation.
Think of it as…
Caring for the patient means also caring for the environment they live in—both inside and outside the hospital walls.
Challenges in Implementing Nightingale’s Environmental Principles Today
Despite the widespread influence of Nightingale’s Environmental Theory, modern healthcare settings face several challenges in consistently applying her principles.
Factors such as resource constraints, technological demands, and overcrowded facilities can complicate efforts to maintain optimal environments for healing.
1) Resource Constraints
In underdeveloped or disaster-affected areas, access to clean water, sanitation, and proper ventilation may be limited, making it difficult to implement Nightingale’s principles effectively.
Example:
Remote clinics in rural areas may lack proper waste disposal systems or clean water, increasing the risk of infection outbreaks.
Nurses often have to improvise and prioritize the most critical measures, such as providing clean drinking water or temporary hygiene stations.
Possible Solution:
Partnerships with organizations specializing in public health infrastructure can help deliver essential resources like mobile water purification units and sanitation kits.
2) Modern Healthcare Technology
While advanced medical equipment improves diagnostic and treatment outcomes, it can sometimes create conflicts with environmental principles, such as generating excessive noise or requiring sterile conditions that limit natural ventilation.
Example:
Operating rooms often rely on artificial ventilation to maintain sterile environments, which limits the use of natural air circulation—a key aspect of Nightingale’s focus on clean air.
Possible Solution:
Balancing high-tech care with environmental factors through noise-reduction strategies, air filtration systems, and quiet, restorative spaces for post-operative recovery.
3) Overcrowded Hospitals
High patient volumes, particularly during crises such as pandemics, can lead to overcrowded wards, making it difficult to maintain cleanliness and adequate ventilation.
Example:
During the COVID-19 pandemic, many hospitals faced overburdened ICUs where maintaining proper sanitation and air quality was a constant challenge.
Possible Solution:
Temporary isolation zones and mobile healthcare units can help reduce patient density and allow proper environmental management.
Nightingale’s Environmental Theory Quiz
1) What did Florence Nightingale believe was essential for recovery and health improvement?
a) Medication
b) Proper sanitation, ventilation, and hygiene
c) Nutritional supplements
d) Constant monitoring of vital signs
2) Which environmental factor did Nightingale emphasize to prevent airborne infections?
a) Clean water
b) Proper lighting
c) Clean air and ventilation
d) Soundproof environments
3) How did Nightingale’s theory address mental health?
a) Through nutrition plans
b) Encouraging family visits
c) Promoting quiet environments and exposure to natural light
d) Frequent counseling
4) Nightingale’s principles are most closely related to which of the following nursing practices?
a) Advanced wound care
b) Infection control and prevention
c) Diagnostic imaging
d) Medication management
5) In modern healthcare, Nightingale’s ideas are applied to:
a) Intensive care units, sanitation protocols, and hospital design
b) Genetic research and DNA sequencing
c) Pharmaceutical manufacturing
d) Data analytics in healthcare
Nightingale’s Environmental Theory Quiz Answers
- Correct Answer: b
- Correct Answer: c
- Correct Answer: c
- Correct Answer: b
- Correct Answer: a
Nightingale’s Environmental Theory Questions and Answers
1) What is the primary focus of Nightingale’s Environmental Theory?
The theory focuses on how environmental factors such as clean air, water, lighting, and sanitation promote health and prevent illness.
2) How can modern nurses implement Nightingale’s ideas in practice?
Nurses can ensure clean environments, proper ventilation, noise reduction, and effective hand hygiene to support recovery and reduce infections.
3) What role does lighting play in patient recovery, according to Nightingale?
Adequate lighting, especially natural light, improves mood, biological functioning, and overall patient recovery.
4) Why is noise control important in healthcare settings?
Noise control minimizes patient stress, promotes rest, and contributes to faster recovery.
5) How does Nightingale’s theory influence infection control protocols today?
Modern infection control measures, such as sanitation, sterile environments, and air filtration systems, are rooted in Nightingale’s emphasis on hygiene and cleanliness.
Conclusion
Florence Nightingale’s Environmental Theory remains a guiding force in modern nursing, with its principles of cleanliness, ventilation, sanitation, and holistic care forming the basis of healthcare standards worldwide.
From infection control protocols to hospital design and patient care practices, her insights continue to save lives and promote healing.
Nightingale understood that nursing is not just about treating diseases but also about creating environments where healing can thrive.
As healthcare faces new challenges like antimicrobial resistance and pandemics, her environmental principles remain as vital as ever.
Final Reflective Question:
How can you integrate Nightingale’s environmental principles into your current nursing practice to improve patient outcomes?