Dorothea Orem, a pioneer in nursing theory, developed the Self-Care Deficit Nursing Theory (SCDNT) to guide nurses in understanding when and how to intervene in patient care.
This theory addresses the gap that arises when individuals are unable to meet their own self-care needs due to illness, injury, or other limitations.
Dorothea Orem’s theory is highly adaptable across different settings, from post-surgical recovery to chronic disease management.
In this guide, we will explore the core concepts, practical applications, and modern implications of the theory, offering examples and tools for effective nursing practice.
What You’ve Learned – Dorothea Orem’s Self-Care Deficit Theory
- Nurses address self-care deficits to promote independence: Orem’s theory highlights when nursing interventions are necessary to support patients who cannot meet their own care needs due to illness or other limitations.
- Three nursing systems guide interventions: Nurses apply the wholly compensatory, partially compensatory, or supportive-educative system based on the patient’s level of dependence and progress toward recovery.
- Basic conditioning factors influence self-care: Personal and environmental factors like age, health status, and social conditions determine how well a patient can meet their self-care requisites.
- Patient education is central to long-term care: The supportive-educative system focuses on teaching and empowering patients to take responsibility for their health, ensuring sustained recovery and management of chronic conditions.
- Orem’s theory remains adaptable in modern healthcare: From post-surgical recovery to chronic disease management, it offers a framework for personalized care that fosters patient autonomy and well-being.
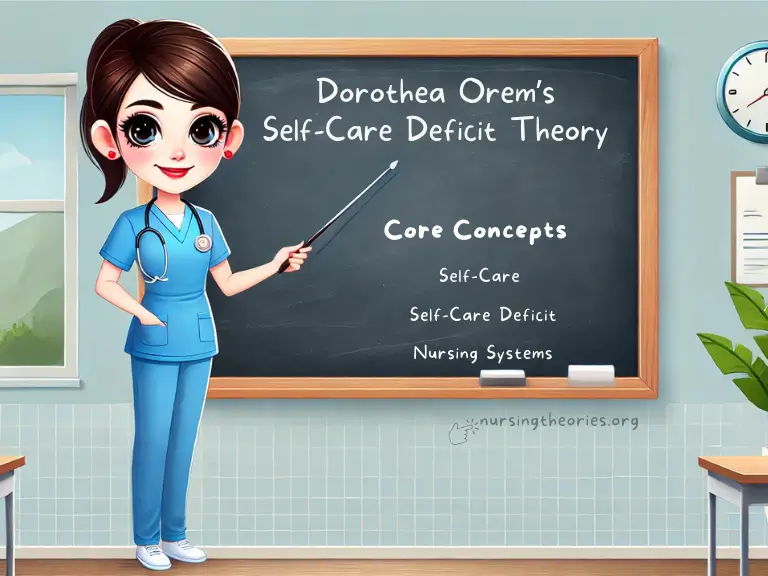
Core Concepts of Dorothea Orem’s Self-Care Deficit Nursing Theory
Orem’s theory is built on the understanding that self-care is a crucial part of maintaining health.
When patients are unable to meet their self-care needs, nurses step in to assist them, with the ultimate goal of restoring their independence.
1) Self-Care
- Definition and importance: Self-care refers to the deliberate activities individuals perform to maintain their health and well-being.
- Why it’s central to Orem’s theory: The theory emphasizes that nursing is necessary when patients cannot perform self-care due to illness or external limitations.
- Example: A diabetic patient practicing daily blood glucose monitoring and adhering to a proper diet demonstrates effective self-care.
Key Insight:
Self-care is a learned behavior, and when patients face barriers, nurses act as temporary or long-term support systems.
Think of it as…
Providing a bridge—nurses help patients cross difficult periods until they can resume self-care on their own.
2) Self-Care Deficit
A self-care deficit occurs when patients cannot meet their own basic or condition-specific needs due to physical, mental, or emotional challenges.
When a deficit occurs:
- Patients may be unable to perform essential tasks such as feeding, dressing, or taking medications.
- The deficit can be temporary or long-term, depending on the nature of the illness or injury.
Example:
A post-surgical patient may experience a temporary self-care deficit, requiring help with bathing, mobility, and wound care.
Key Insight:
Recognizing the type and extent of the self-care deficit allows nurses to create targeted, effective care plans.
Think of it as…
Identifying gaps in a puzzle where nursing interventions fit perfectly to restore the complete picture of patient independence.
3) Nursing Systems
Orem’s theory outlines three nursing systems based on the patient’s level of dependence and the extent of their self-care deficit:
1) Wholly Compensatory System:
- Nurses provide complete care when the patient is unable to perform any self-care activities independently.
- Example: Patients in the ICU who require full assistance for hygiene, feeding, and mobility.
2) Partially Compensatory System:
- The patient can perform some self-care tasks but requires assistance with others.
- Example: A stroke patient who can brush their teeth but needs help dressing and walking.
3) Supportive-Educative System:
- The patient is capable of self-care but lacks knowledge or confidence. Nurses provide guidance and teaching.
- Example: A newly diagnosed diabetic patient learning to administer insulin and manage blood glucose levels.
Key Insight:
Understanding the appropriate nursing system helps tailor interventions to maximize patient independence.
Think of it as…
Adjusting the level of support based on the patient’s progress, like training wheels on a bicycle that are gradually removed.
Understanding the Self-Care Deficit Components in Detail
Orem’s Self-Care Deficit Theory includes several key components that help nurses assess patients’ needs and develop personalized care plans.
These components guide the identification of self-care deficits and the necessary interventions.
1) Basic Conditioning Factors
Definition:
Basic conditioning factors refer to the individual characteristics and circumstances that influence a person’s ability to engage in self-care.
Key Factors Include:
- Age
- Gender
- Developmental stage
- Health status (acute or chronic)
- Socioeconomic conditions
- Environment
Example:
An elderly patient with arthritis may struggle to meet hygiene and dressing needs due to joint pain and reduced mobility.
Key Insight:
Assessing conditioning factors allows nurses to understand why a self-care deficit exists and develop interventions tailored to the patient’s situation.
Think of it as…
Identifying the obstacles on a patient’s path and clearing the way to independence.
2) Therapeutic Self-Care Demand
Definition:
This refers to the total amount of self-care a patient needs to maintain or restore health, which varies based on their condition.
Practical Consideration:
The demand includes tasks like medication administration, hygiene, wound care, and mental health management.
Nurses must evaluate whether the patient can meet these demands independently or requires assistance.
Example:
A patient recovering from a heart attack may have therapeutic self-care demands related to diet modification, physical activity, and stress management.
Key Insight:
Understanding the therapeutic self-care demand helps nurses prioritize which tasks require immediate intervention.
Think of it as…
A checklist of health tasks that nurses help patients address one step at a time.
3) Self-Care Requisites
Orem categorizes self-care requisites into three groups, each addressing specific needs:
1) Universal Self-Care Requisites:
- These are basic needs that apply to all individuals, such as breathing, eating, elimination, and maintaining safety.
- Example: Ensuring a patient with pneumonia maintains adequate oxygenation through respiratory support.
2) Developmental Self-Care Requisites:
- These relate to the needs that arise during different life stages, such as infancy, adolescence, or old age.
- Example: A newborn requires feeding and temperature regulation until they develop these abilities independently.
3) Health Deviation Self-Care Requisites:
- These arise when a patient’s health is compromised by illness or injury.
- Example: A patient with diabetes needs to monitor blood glucose levels and adhere to a specific diet.
Key Insight:
Addressing the appropriate requisites ensures comprehensive care, targeting both immediate and long-term health needs.
Think of it as…
Covering all bases—nurses address basic, developmental, and illness-specific needs to support holistic recovery.
Real-World Applications of Dorothea Orem’s Theory
Orem’s Self-Care Deficit Theory is highly practical and applicable across various healthcare settings.
Nurses frequently apply this framework to help patients regain their independence, whether they are recovering from surgery, managing chronic illnesses, or learning new self-care routines.
Case Study 1: Post-Surgical Recovery
Scenario: A 50-year-old male patient undergoes abdominal surgery and experiences pain, weakness, and limited mobility, making it difficult to bathe, dress, or walk independently.
Application of Orem’s Theory:
- Nursing System: Wholly Compensatory System
- Interventions: Nurses provide full assistance with daily hygiene, dressing, and mobility until the patient gradually regains strength.
- Self-Care Deficit: Temporary inability to meet basic hygiene and mobility needs due to post-surgical weakness.
Outcome: The nurse gradually transitions the patient to a partially compensatory system, supporting him during rehabilitation exercises and encouraging independent walking as strength returns.
Case Study 2: Chronic Disease Management
Scenario: A 45-year-old woman is diagnosed with type 2 diabetes and initially struggles to manage her diet, medication, and blood glucose monitoring.
Application of Orem’s Theory:
- Nursing System: Supportive-Educative System
- Interventions: The nurse provides educational sessions on proper insulin administration, diet planning, and recognizing symptoms of high or low blood sugar.
- Self-Care Deficit: Lack of knowledge and experience in managing the disease.
Outcome: The patient gradually gains confidence and competence in managing her condition, reducing the need for regular nursing intervention.
Case Study 3: Pediatric Care
Scenario: An 8-year-old boy with asthma requires regular medication and breathing exercises to manage his symptoms.
His parents report difficulty in ensuring the child adheres to his treatment plan.
Application of Orem’s Theory:
- Nursing System: Partially Compensatory System (parents provide partial assistance)
- Interventions: The nurse works with both the child and his parents to develop a routine that includes using an inhaler correctly and performing breathing exercises.
- Self-Care Deficit: The child’s developmental stage and lack of understanding of his condition limit his ability to independently manage asthma.
Outcome: With parental support and education, the child learns to monitor his symptoms and use his inhaler independently.
Key Insight:
Real-world applications of Orem’s theory demonstrate how tailored nursing interventions can promote patient autonomy and long-term health improvements.
Think of it as…
Guiding patients through recovery or management in stages, from dependency to full independence.
Modern Implications of Dorothea Orem’s Theory
Orem’s Self-Care Deficit Theory remains highly relevant in modern healthcare, particularly as patient-centered care, chronic disease management, and interdisciplinary collaboration become essential.
Her framework supports not only acute interventions but also long-term strategies that empower patients.
1) Importance in Chronic Care and Rehabilitation
Chronic conditions like diabetes, hypertension, and heart disease require consistent self-care practices.
Orem’s theory helps nurses develop plans to guide patients through gradual transitions from wholly or partially compensatory systems to supportive-educative systems, promoting long-term independence.
Example:
A patient recovering from a stroke may initially require full assistance with mobility, but over time, rehabilitation programs can help them regain independence with walking and daily activities.
Key Insight:
Patients benefit from gradual, goal-oriented care plans that enable them to manage their conditions independently.
Think of it as…
Helping patients climb a staircase where each step represents incremental progress toward independence.
2) Emphasis on Patient Education
Patient education is central to Orem’s theory, particularly within the supportive-educative system.
Educating patients about their conditions, medications, and lifestyle adjustments equips them to maintain their health independently.
Example:
A newly diagnosed heart failure patient is taught how to monitor fluid intake, recognize signs of worsening symptoms, and follow a low-sodium diet.
Key Insight:
Knowledge empowers patients to take ownership of their care, reducing hospital readmissions and improving long-term outcomes.
Think of it as…
Giving patients the tools they need to be their own caregivers.
3) Integration with Interdisciplinary Teams
Modern healthcare often involves collaboration among various professionals, such as physical therapists, dietitians, and social workers.
Orem’s theory complements this approach by ensuring that nurses work with other disciplines to meet all aspects of a patient’s self-care needs.
Example:
A patient with mobility issues may work with a nurse for hygiene needs, a physical therapist for movement improvement, and a dietitian for nutritional support.
Key Insight:
Interdisciplinary teams offer comprehensive care, ensuring that patients receive support for both physical and emotional needs.
Think of it as…
A well-oiled machine where every part contributes to the patient’s holistic recovery.
Challenges and Limitations of Orem’s Theory
While Orem’s Self-Care Deficit Theory provides a valuable framework for patient-centered care, its application can face challenges, especially in complex or resource-limited healthcare environments.
Recognizing and addressing these limitations helps nurses optimize their practice.
1) Complexity in Managing Multiple Deficits
Patients with comorbidities or severe conditions often present overlapping self-care deficits, making it difficult for nurses to prioritize interventions.
For example, a patient recovering from surgery may also have diabetes and hypertension, each requiring distinct nursing interventions.
Example:
A patient with a hip fracture who is also undergoing dialysis may require assistance with mobility, dietary management, and fluid regulation.
Key Insight:
Nurses need to conduct comprehensive assessments and collaborate with interdisciplinary teams to manage multiple deficits effectively.
Think of it as…
Juggling multiple tasks where careful prioritization ensures no critical need is overlooked.
2) Resource Limitations and Staffing Shortages
In resource-limited settings, nurses may face time constraints and high patient-to-nurse ratios, which can limit their ability to provide individualized care.
Meeting all of a patient’s self-care requisites may not always be feasible in these environments.
Example:
In a busy hospital ward, a nurse may have to prioritize immediate physical needs like medication administration and delay addressing long-term self-care education.
Key Insight:
Even small interventions can promote progress—nurses can address key deficits efficiently and provide follow-up support when resources allow.
Think of it as…
Watering plants selectively to ensure all essential areas get the attention they need, even in limited time.
3) Adapting to Technology
Technological advancements like remote monitoring, electronic health records, and telehealth have streamlined some aspects of nursing care.
However, they may also reduce face-to-face interaction, which is essential for effective assessment and emotional support.
Example:
A home health nurse may rely on digital monitoring tools to check a patient’s blood pressure or glucose levels but may miss important cues like anxiety or confusion without direct interaction.
Key Insight:
Balancing technology with hands-on care ensures that nurses maintain a holistic view of their patients’ needs.
Think of it as…
Using technology as a supplement, not a replacement, for personalized care.
Dorothea Orem’s Self-Care Deficit Theory Quiz
1) When does a self-care deficit occur, according to Orem’s theory?
a) When a patient is experiencing emotional distress
b) When a patient cannot meet their own self-care needs
c) When a patient is dependent on medical devices
d) When a patient has a chronic condition
2) Which nursing system would be applied to a patient who can perform some self-care activities but still requires assistance?
a) Wholly compensatory system
b) Partially compensatory system
c) Supportive-educative system
d) Therapeutic self-care system
3) Which of the following is an example of a developmental self-care requisite?
a) Maintaining proper nutrition
b) Supporting a child’s emotional growth
c) Providing oxygen therapy
d) Assisting with wound care
4) How does the supportive-educative system help patients regain independence?
a) By performing all care tasks for the patient
b) By monitoring the patient’s condition remotely
c) By educating and guiding patients in performing their own care
d) By administering medications regularly
5) Which of the following best explains Orem’s concept of basic conditioning factors?
a) The minimum amount of care needed for recovery
b) Environmental and personal factors that influence self-care abilities
c) Physical therapy programs for regaining mobility
d) Psychological interventions aimed at emotional healing
Dorothea Orem’s Self-Care Deficit Theory Quiz Answers with Rationale
1) Correct Answer: b) When a patient cannot meet their own self-care needs
Rationale: Orem’s theory defines a self-care deficit as occurring when individuals are unable to perform self-care actions due to illness, injury, or external factors.
2) Correct Answer: b) Partially compensatory system
Rationale: The partially compensatory system applies when patients can perform some but not all self-care tasks, requiring nurses to assist as needed.
3) Correct Answer: b) Supporting a child’s emotional growth
Rationale: Developmental self-care requisites address needs related to life stages, such as emotional and social development in children.
4) Correct Answer: c) By educating and guiding patients in performing their own care
Rationale: In the supportive-educative system, nurses focus on teaching and supporting patients to regain independence by understanding and managing their own care needs.
5) Correct Answer: b) Environmental and personal factors that influence self-care abilities
Rationale: Basic conditioning factors include elements such as age, gender, environment, and health status, which impact a patient’s ability to perform self-care.
Questions and Answers of Dorothea Orem’s Self-Care Deficit Theory
1) Q: What is the primary purpose of Dorothea Orem’s Self-Care Deficit Nursing Theory?
A: To identify when patients are unable to meet their own self-care needs and guide nursing interventions accordingly.
2) Q: How do nurses determine which self-care requisites are unmet?
A: Through patient assessments, observation, and understanding the patient’s medical history and current condition.
3) Q: What role do basic conditioning factors play in the theory?
A: They help nurses identify the underlying reasons for a self-care deficit, such as age, health status, or socioeconomic conditions.
4) Q: Why is the supportive-educative system critical for long-term care?
A: It focuses on teaching patients self-care skills, promoting long-term independence and better health outcomes.
5) Q: How can Orem’s theory be applied in chronic disease management?
A: By developing personalized care plans that guide patients through education, partial assistance, and ultimately self-management.
Conclusion
Dorothea Orem’s Self-Care Deficit Nursing Theory offers a comprehensive framework for understanding and addressing patients’ self-care needs.
By identifying self-care deficits and categorizing them into different nursing systems, nurses can provide personalized care that promotes patient autonomy, recovery, and well-being.
The theory’s emphasis on education and collaboration also ensures its relevance in modern healthcare, from chronic care to rehabilitation.
Whether dealing with temporary deficits or long-term conditions, Dorothea Orem’s theory guides nurses in creating practical, goal-oriented interventions that adapt to each patient’s unique circumstances.
Final Reflective Question: How can you incorporate Dorothea Orem’s Self-Care Deficit Theory into your daily nursing practice to foster patient independence and long-term success?