Patricia Benner, a renowned nurse theorist and educator, profoundly influenced nursing education and practice with her From Novice to Expert Theory.
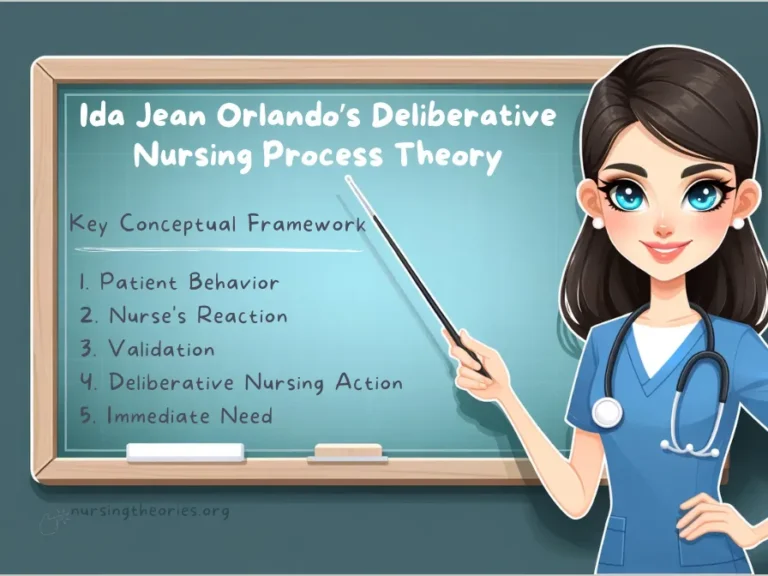
This theory provides a framework for understanding how nurses acquire skills, develop expertise, and evolve through five distinct stages based on experience and clinical exposure.
Benner’s model shifted the focus from knowledge acquisition through formal instruction to experiential learning gained at the bedside.
Explore more about her contributions to nursing here.
This article explores Benner’s nursing theory, examining its principles, strategies, and impact on nursing practice.
What You’ve Learned – Patricia Benner’s From Novice to Expert Theory
- The Five Stages of Nursing Expertise: The theory defines five stages: novice, advanced beginner, competent, proficient, and expert. As nurses progress through these stages, they transition from relying on rigid guidelines to making intuitive, experience-based decisions.
- The Importance of Clinical Experience: Experience in real-world clinical settings is key to progressing through the stages. Nurses learn through exposure to varied patient cases, which enhances their decision-making and pattern recognition.
- Mentorship and Reflection: Mentorship is vital to help nurses progress from novice to expert. Guidance from more experienced colleagues, coupled with self-reflection, accelerates professional development and improves clinical judgment.
- The Role of Intuition in Expert Practice: As nurses gain expertise, they develop intuitive decision-making skills. This is a critical aspect of expert practice, allowing nurses to act swiftly and effectively in complex situations.
- Practical Implications for Nursing Education: Benner’s theory highlights the need for experiential learning in nursing education, emphasizing the value of real-world experience and reflective practice to enhance nurses’ clinical expertise and improve patient care.
Core Concepts of Patricia Benner’s From Novice to Expert Theory
Benner’s theory identifies five progressive stages of nursing expertise, emphasizing that clinical experience, reflection, and mentorship are essential for transitioning from a novice nurse to an expert.
These stages highlight the evolving nature of decision-making, knowledge integration, and intuition in nursing.
Stage 1: Novice
Novices rely on rules, guidelines, and protocols to perform tasks since they lack experience.
Their focus is on learning how to execute instructions rather than understanding the broader context of care.
Example: A nursing student administering medication follows a step-by-step checklist but may not fully grasp the implications of medication errors.
Stage 2: Advanced Beginner
At this stage, nurses begin to recognize recurring patterns based on limited experience.
Although they still rely on guidelines, they can identify key aspects of clinical situations and require less supervision.
Example: A newly graduated nurse recognizes that a patient experiencing shortness of breath and elevated heart rate may need immediate intervention.
Stage 3: Competent
Competent nurses have 2-3 years of clinical experience and can prioritize tasks and make decisions based on clinical reasoning.
They develop plans of care with greater confidence and efficiency.
Example: A nurse in a medical-surgical unit efficiently manages multiple patients, prioritizing pain management for one while monitoring vital signs for another.
Stage 4: Proficient
Proficient nurses view situations holistically and can anticipate patient needs based on their clinical understanding.
Their decision-making becomes more intuitive, and they can adapt care plans to changing situations.
Example: A proficient nurse in the ICU recognizes subtle signs of sepsis, such as confusion or changes in skin tone, even before lab results confirm the diagnosis.
Stage 5: Expert
Expert nurses demonstrate intuitive grasp and deep understanding of clinical situations without needing to rely on rules or guidelines.
Their actions are based on extensive experience and reflective practice.
Example: An expert emergency room nurse detects life-threatening conditions like internal bleeding by observing minor changes in the patient’s condition, acting swiftly to initiate care.
Key Insight: Progression through the stages is not automatic; it requires continuous exposure to clinical experiences and reflective learning.
Think of it as… Climbing a ladder, where each step builds on the previous one, leading to greater independence, judgment, and expertise.
The Role of Clinical Experience in Learning
In Patricia Benner’s From Novice to Expert Theory, clinical experience is essential to moving from beginner-level competency to intuitive expertise.
Experience bridges the gap between theoretical knowledge and practical application, allowing nurses to develop critical thinking, pattern recognition, and situational awareness.
How Clinical Experiences Shape Expertise
Through continuous exposure to real-world situations, nurses refine their decision-making and develop the ability to predict outcomes based on previous encounters.
Experience also helps nurses shift from rigid rule-following to adaptable, intuitive responses.
Example: A novice nurse following a checklist may take time to recognize early signs of respiratory distress.
However, with experience in similar cases, the same nurse can anticipate complications like declining oxygen levels based on subtle changes in the patient’s breathing.
Key Insight: As nurses gain experience, they no longer rely solely on instructions—they develop an internal sense of how to handle situations based on what they’ve learned in practice.
Think of it as… Learning to cook a complex recipe.
At first, you measure every ingredient precisely, but with practice, you rely on taste and intuition to create the perfect dish.
The Role of Mentorship and Feedback
Guidance from proficient or expert nurses accelerates the development of less experienced nurses.
Mentors offer feedback on clinical decisions, helping novices reflect on their actions and refine their practice.
Example: A novice nurse in a busy emergency unit may initially struggle with prioritizing care, but an experienced mentor can provide tips on recognizing life-threatening symptoms and managing tasks efficiently.
Key Insight: Mentorship facilitates growth by offering real-time advice, helping novice nurses progress faster through the stages of Benner’s theory.
Think of it as… A sports coach offering insights after a game, showing players what worked, what didn’t, and how to improve.
Integrating Knowledge, Skills, and Intuition
One of the key contributions of Patricia Benner’s theory is the emphasis on integrating formal knowledge, practical skills, and intuitive understanding in nursing practice.
As nurses move through the stages of development, they become better at combining what they’ve learned in the classroom with what they’ve experienced at the bedside.
How Knowledge and Experience Interact
Knowledge provides the foundation for safe and effective practice, but it is only through repeated application that nurses develop the confidence to adapt their care based on patient needs.
With experience, nurses shift from rigid application of facts to making complex decisions guided by both logic and intuition.
Example: A competent nurse managing a diabetic patient initially relies on protocols for monitoring blood sugar.
However, after managing several similar cases, the same nurse intuitively anticipates complications, such as hypoglycemia, and preemptively adjusts the care plan before a crisis occurs.
Key Insight: Intuition isn’t guesswork—it’s the result of accumulated experience and deep understanding of patient care.
Think of it as… Learning to ride a bike.
At first, you rely on training wheels and balance tips, but over time, you instinctively adjust your movements without needing to think about every step.
The Balance Between Technical Knowledge and Practical Intuition
Experienced nurses demonstrate an effective balance of both evidence-based practice and intuitive action.
They can adapt their responses in emergencies and other dynamic situations where strict guidelines might not fully apply.
Example: An expert nurse in the ICU quickly recognizes that a patient’s subtle agitation may indicate deteriorating oxygenation, even before lab results confirm it.
The nurse intuitively prepares for interventions, preventing further complications.
Key Insight: The ability to balance clinical knowledge with real-time judgment leads to proactive, rather than reactive, patient care.
Think of it as… Being a skilled pilot who uses both flight instruments and gut instinct to navigate turbulence safely.
Applying Benner’s Theory through the Nursing Process
Patricia Benner’s From Novice to Expert Theory integrates seamlessly with the nursing process, guiding how nurses at different stages assess, plan, implement, and evaluate patient care.
As nurses progress in their expertise, their approach to each step of the nursing process evolves to reflect their level of competence and decision-making ability.
Step 1: Assessment and Recognizing Patterns
Nurses assess patient conditions through observations, vital signs, and communication.
Novices rely on structured checklists, while more experienced nurses identify patterns and potential complications based on previous cases.
Example: A novice nurse caring for a post-operative patient might follow a checklist to monitor pain and wound drainage, while a proficient nurse immediately recognizes abnormal signs such as increasing pain or changes in wound color, indicating possible infection.
Key Insight: As nurses gain experience, they shift from task-oriented assessments to recognizing broader patterns that inform care decisions.
Think of it as… Moving from assembling a puzzle piece by piece to seeing how the entire picture fits together at a glance.
Step 2: Diagnosis and Clinical Reasoning
Diagnosis involves identifying patient problems based on data collected during the assessment.
Nurses at different stages approach diagnosis differently—novices focus on textbook definitions, while experienced nurses combine clinical data with their intuitive understanding of patient conditions.
Example: A competent nurse identifies that a patient’s shortness of breath and fatigue may indicate heart failure, but an expert nurse anticipates worsening symptoms based on subtle changes in the patient’s posture and skin tone.
Key Insight: With experience, nurses improve their clinical reasoning and can make more accurate, timely diagnoses
Step 3: Planning and Goal-Setting
Planning involves creating a care plan with specific, achievable goals tailored to the patient’s condition.
Novices may focus on following predefined care pathways, while more experienced nurses consider individual patient needs and potential challenges.
Example: A novice nurse caring for a diabetic patient might create a goal to maintain blood glucose levels within a specific range, strictly following standard protocols.
In contrast, a proficient nurse considers the patient’s diet, exercise habits, and emotional readiness before setting personalized goals, such as gradually reducing carbohydrate intake or encouraging short daily walks.
Key Insight: Experienced nurses design flexible care plans that balance clinical guidelines with personalized patient needs.
Think of it as… Planning a trip—novices follow a set itinerary, while experts adjust plans based on real-time conditions like weather or traffic.
Step 4: Implementation and Adaptability
The implementation stage involves carrying out the care plan and adapting interventions as needed.
Novices tend to stick rigidly to the plan, while experienced nurses adjust on the spot based on the patient’s response.
Example: A novice nurse assisting a post-surgical patient may follow the care plan exactly, administering pain medication at scheduled intervals.
Meanwhile, a proficient nurse observes the patient’s discomfort, consults the pain chart, and adjusts the intervention to provide relief sooner if necessary.
Key Insight: Implementation is dynamic—experienced nurses can modify actions in real time to improve outcomes.
Think of it as… Following a recipe where expert chefs taste as they cook, adjusting seasonings based on flavor rather than rigidly following measurements.
Step 5: Evaluation and Reflective Learning
Evaluation involves assessing whether the patient’s condition is improving and determining whether adjustments to the care plan are needed.
While novices evaluate outcomes based on preset criteria, experts reflect on broader aspects, such as patient satisfaction, emotional well-being, and long-term progress.
Example: A novice nurse may evaluate a patient’s wound healing by checking for signs of infection, while an expert nurse evaluates not only physical healing but also the patient’s emotional state, pain management, and understanding of aftercare instructions.
Key Insight: Experienced nurses go beyond evaluating immediate outcomes—they reflect on how the entire care process can be improved for future cases.
Think of it as… Reviewing a performance—novices check whether they hit the right notes, while experts reflect on how to make the overall experience better.
Case Studies Demonstrating Benner’s From Novice to Expert Theory
Case Study 1: A Novice Nurse Managing a Post-Surgical Patient
A newly graduated nurse, Sarah, was assigned to care for a patient recovering from abdominal surgery.
With limited clinical experience, Sarah followed the care plan strictly, using a checklist to monitor vital signs, administer medications, and assess the surgical wound.
However, when the patient reported discomfort and a slight fever, Sarah delayed intervention, unsure whether it warranted immediate action.
After consulting her supervisor, she realized that the fever and discomfort were early signs of infection.
Key Insight: Novices rely heavily on structured guidelines and benefit from mentorship to help them build confidence and improve their critical thinking skills.
Case Study 2: An Advanced Beginner Recognizing Patterns in Diabetic Care
Michael, an advanced beginner with six months of experience, was monitoring a diabetic patient admitted for high blood sugar levels.
During his shift, the patient complained of dizziness and fatigue, which Michael recognized from prior cases as signs of impending hypoglycemia.
He quickly checked the patient’s blood glucose levels and provided juice to stabilize them before further complications occurred.
Key Insight: Advanced beginners can identify recurring patterns, reducing their dependence on strict protocols and improving patient outcomes.
Case Study 3: An Expert Nurse Managing Critical Care
Jessica, an expert nurse in the ICU, was assigned to care for a patient with sepsis.
Without waiting for lab results, she identified signs of deteriorating oxygenation based on the patient’s subtle restlessness and slightly increased respiratory rate.
Drawing from her extensive experience, Jessica immediately initiated oxygen support and alerted the medical team.
Her quick intervention prevented the patient’s condition from worsening.
Key Insight: Expert nurses rely on intuitive decision-making and a deep understanding of patient care, allowing them to anticipate and prevent complications.
Modern Implications of Benner’s Theory in Nursing Practice
Patricia Benner’s From Novice to Expert Theory continues to be a valuable framework in modern nursing practice.
With increasing emphasis on patient-centered care, interprofessional collaboration, and evidence-based practice, Benner’s model aligns with today’s healthcare needs by emphasizing the evolution of clinical expertise.
Guiding Professional Development and Continuing Education
Benner’s theory provides a roadmap for nursing education and professional development.
By recognizing the distinct stages of expertise, educators can design targeted curricula that support nurses in progressing from novices to experts.
This approach encourages lifelong learning and ensures that nurses continuously build on their clinical knowledge and skills.
Example: Nursing schools and continuing education programs can tailor courses to address the specific needs of nurses at each stage of expertise, fostering a supportive learning environment.
Key Insight: The theory promotes tailored professional development strategies that align with a nurse’s stage of expertise, ensuring they receive the support they need to advance in their careers.
Think of it as… A coach guiding a player through different levels of a game—beginning with fundamental skills and progressing toward advanced strategies as the player gains experience.
Enhancing Clinical Decision-Making
The ability to make informed, accurate clinical decisions improves as nurses gain experience.
Benner’s theory highlights how clinical judgment evolves over time, moving from reliance on protocols and checklists to intuitive decision-making based on past experiences.
This shift in clinical decision-making not only enhances patient care but also leads to more efficient and effective practice.
Example: Expert nurses can make decisions in high-pressure situations—such as recognizing the early signs of sepsis—without needing to refer to guidelines, drawing on years of accumulated clinical knowledge.
Key Insight: As nurses progress through the stages, their clinical judgment becomes more nuanced, leading to faster and more accurate decision-making.
Think of it as… A chess master who anticipates multiple moves ahead, informed by experience, rather than focusing solely on each individual move.
Improving Patient Outcomes
Benner’s theory emphasizes that as nurses gain experience, they improve not only their clinical skills but also their ability to deliver holistic care.
Nurses at the proficient and expert stages are better at anticipating patient needs, which leads to improved outcomes and higher patient satisfaction.
By applying Benner’s theory, healthcare systems can ensure that care is timely, accurate, and tailored to each patient’s unique needs.
Example: In a surgical unit, expert nurses recognize early signs of post-operative complications, allowing them to take preventative action before issues arise.
Key Insight: With experience, nurses can anticipate problems before they occur, enhancing patient safety and satisfaction.
Think of it as… A seasoned firefighter who can quickly assess danger and take action to prevent a disaster, relying on years of training and experience.
Challenges and Limitations of Benner’s Theory
While Patricia Benner’s From Novice to Expert Theory has been widely influential, its application in nursing practice is not without challenges.
Several factors, including variability in progression, differing experiences across specialties, and resource limitations, can impact the effectiveness of the model in real-world settings.
Variability in Progression
One of the challenges of applying Benner’s theory is the variability in how nurses progress through the stages.
Not all nurses move from novice to expert at the same pace due to individual differences, exposure to clinical experiences, and the types of mentorship they receive.
Some nurses may progress more quickly, while others may need more time to develop the necessary skills and confidence.
Example: A nurse in a busy emergency department may gain exposure to a wide range of cases, helping them advance to the competent stage more quickly.
In contrast, a nurse in a more routine, specialized setting may not encounter enough varied situations to progress as rapidly.
Key Insight: While Benner’s theory provides a useful framework, it’s important to remember that progression through the stages is individualized and may vary based on context.
Think of it as… Different students learning at different speeds, even though they’re all taking the same course, because they have different learning styles and experiences.
Limited Transferability Across Specialties
Benner’s theory primarily focuses on general nursing practice, and applying it across specialties can be challenging.
The progression from novice to expert may look different in specialized fields such as pediatrics, oncology, or critical care, where nurses face more specific, technical challenges.
Example: A nurse specializing in oncology may need to develop expertise in chemotherapy administration, patient support during treatment, and understanding cancer pathology.
However, in a surgical unit, nurses may be focusing on wound care, post-operative recovery, and anesthesia management.
Key Insight: Benner’s theory should be adapted to accommodate the unique demands and learning opportunities within different nursing specialties.
Think of it as… Different professions—such as teaching, accounting, and healthcare—each requiring specific expertise, but the fundamental learning process is similar.
Overreliance on Experience
While clinical experience is essential for moving through the stages, overreliance on intuition can be problematic if not balanced with evidence-based practice.
Nurses at advanced stages of expertise may sometimes rely too heavily on their gut feelings, leading to potential oversights or errors, especially in complex cases where clinical intuition may not be enough.
Example: An expert nurse might quickly recognize the symptoms of dehydration based on previous experiences.
However, without checking the patient’s laboratory values, they may miss subtle signs of a different condition that presents similarly.
Key Insight: While experience is invaluable, it should always be balanced with ongoing education, evidence-based practices, and peer review to ensure the highest standard of care.
Think of it as… A seasoned driver who, while very experienced, might still occasionally overlook a road sign or traffic signal—relying on experience but needing to stay mindful of new information.
Patricia Benner’s From Novice to Expert Theory Quiz
1) What is the primary focus of Patricia Benner’s From Novice to Expert Theory?
a) The stages of professional development in nursing
b) The development of leadership in nursing
c) The technical skills required for specific procedures
d) The theoretical understanding of patient care
2) In Benner’s model, which stage involves a nurse primarily relying on rules and protocols?
a) Expert
b) Competent
c) Novice
d) Proficient
3) What differentiates an advanced beginner from a novice nurse in Benner’s theory?
a) Advanced beginners can work independently without guidance
b) Advanced beginners begin to recognize recurring patterns based on experience
c) Advanced beginners prioritize patient outcomes over tasks
d) Advanced beginners have fully mastered their role
4) How does an expert nurse differ from a proficient nurse?
a) Experts rely more heavily on protocols
b) Experts make decisions quickly based on intuition and extensive experience
c) Experts focus more on patient comfort than clinical outcomes
d) Experts need to gather more data before making decisions
5) Which factor is essential for a nurse’s progression from novice to expert, according to Benner?
a) More formal education and theoretical learning
b) Consistent, diverse clinical experience and reflection
c) Strong management skills
d) Reduced patient interaction
Patricia Benner’s From Novice to Expert Theory Quiz Answers with Rationale
- Correct Answer: a) The stages of professional development in nursing
Rationale: Benner’s theory focuses on how nurses develop through five stages, from novice to expert, and how their clinical skills and decision-making evolve with experience. - Correct Answer: c) Novice
Rationale: Novice nurses rely on rules and guidelines, as they lack the experience to make intuitive decisions or recognize patterns in patient care. - Correct Answer: b) Advanced beginners begin to recognize recurring patterns based on experience
Rationale: As nurses progress from novice to advanced beginner, they start to recognize patterns in patient care, which allows them to make more informed decisions. - Correct Answer: b) Experts make decisions quickly based on intuition and extensive experience
Rationale: Expert nurses rely on their extensive experience and intuition to make decisions quickly and effectively, whereas proficient nurses are still refining their decision-making processes. - Correct Answer: b) Consistent, diverse clinical experience and reflection
Rationale: Progressing from novice to expert relies heavily on ongoing clinical experience and the ability to reflect on practice, leading to improved judgment and decision-making skills.
Questions and Answers on Benner’s From Novice to Expert Theory
Q1: What is the main goal of Benner’s theory?
A: To understand how nurses develop their clinical expertise over time through experiential learning.
Q2: How can mentorship help nurses progress through the stages of Benner’s theory?
A: Mentorship provides guidance, feedback, and opportunities for reflection, helping nurses develop their skills and move toward proficiency and expertise.
Q3: Why do nurses at the expert stage rely on intuition?
A: Expert nurses rely on intuition developed through years of clinical experience, which allows them to make quick, effective decisions without needing to consult guidelines.
Q4: How does Benner’s theory inform nursing education and professional development?
A: The theory emphasizes the importance of experiential learning and mentorship, guiding educators to design curricula and training programs that support the progression of nursing skills over time.
Q5: What is a limitation of relying on intuition in nursing practice?
A: While intuition is helpful, it should be balanced with evidence-based practice to ensure the best outcomes for patients and avoid potential errors in judgment.
Conclusion of Patricia Benner’s From Novice to Expert Theory
Patricia Benner’s From Novice to Expert Theory offers a comprehensive framework for understanding how nurses develop their expertise over time.
Through five distinct stages—novice, advanced beginner, competent, proficient, and expert—nurses progress from relying on rules and protocols to making intuitive, confident decisions based on extensive clinical experience.
This progression emphasizes the value of mentorship, experiential learning, and continuous self-reflection in nursing practice. Learn more about Patricia Benner’s contributions to nursing here.
Final Reflective Question: How can nursing educators and leaders create environments that foster experiential learning and mentorship to help nurses progress from novice to expert?